A Game-Changer for Millions
Ayushman Bharat, through its flagship initiatives – Health and Wellness Centres (HWCs) and the Pradhan Mantri Jan Arogya Yojana (PM-JAY) – has reshaped healthcare in India. A recent study has highlighted PM-JAY’s transformative impact on cancer treatment.
By Dr Suneela Garg & Dr Arvind Garg

Ayushman Bharat, a flagship initiative by the Government of India, was launched following the recommendations of the National Health Policy 2017 to realise the vision of Universal Health Coverage (UHC). This landmark scheme underscores the commitment to Sustainable Development Goals (SDGs) and embodies the principle of “leaving no one behind.”
Introduced in 2018 as the Pradhan Mantri Jan Arogya Yojana (PM-JAY), Ayushman Bharat has revolutionised access to healthcare for economically vulnerable populations in India. The programme provides health insurance coverage of up to INR 5 lakh annually for secondary and tertiary care hospitalisations. Covering over 10 crore families, it stands as the world’s largest government-funded healthcare initiative, making quality treatment accessible to millions.
By alleviating the burden of out-of-pocket medical expenses—an issue that had previously pushed 7 per cent of India’s population into poverty, as noted by NITI Aayog—Ayushman Bharat has become a beacon of hope for many. Offering cashless treatment at empanelled hospitals, it has fostered significant digital transformation in healthcare financing. Automated systems have streamlined billing processes, reduced manual errors, and enhanced overall efficiency.
As of March 2023, over 23.3 crore beneficiaries had enrolled in the scheme, with 4.49 crore hospital admissions recorded. These numbers reflect Ayushman Bharat’s pivotal role in setting new benchmarks for equitable healthcare access.
However, challenges persist. Issues such as delays in payments to healthcare providers, high claim rejection rates, and supply chain inefficiencies necessitate improvements in management systems. To address these gaps, innovations like automated claims processing and digital dashboards are being implemented to ensure timely settlements and minimise disruptions. Despite these challenges, Ayushman Bharat has inspired similar initiatives at the state level. Scaling the programme across India demands robust collaboration among stakeholders, including healthcare providers, insurers, tech enablers, and patients.
The Indian government’s growing commitment to universal healthcare is evident in its increasing expenditure. Health spending rose to 1.9 per cent of GDP in 2023-24 from 1.13 per cent in 2015-16, aligning with the National Health Policy’s target of 2.5 per cent by 2025. This investment is crucial as India’s healthcare sector is expected to reach USD 638 billion by 2025. Ayushman Bharat plays an instrumental role in bridging gaps between affordability and accessibility in this rapidly expanding sector.

Ayushman Bharat marks a shift from a fragmented, sectoral approach to a comprehensive, need-based model of healthcare service delivery. It seeks to address the healthcare system holistically, focusing on prevention, promotion, and ambulatory care across primary, secondary, and tertiary levels.
The scheme adopts a continuum-of-care approach through its two key components:
Health and Wellness Centres (HWCs): These centres provide preventive, promotive, and primary healthcare services to communities.
Pradhan Mantri Jan Arogya Yojana (PM-JAY): This component ensures financial protection for hospital-based care, particularly for the economically disadvantaged.
Ayushman Bharat remains a cornerstone of India’s healthcare transformation, setting the stage for a more equitable and inclusive future.
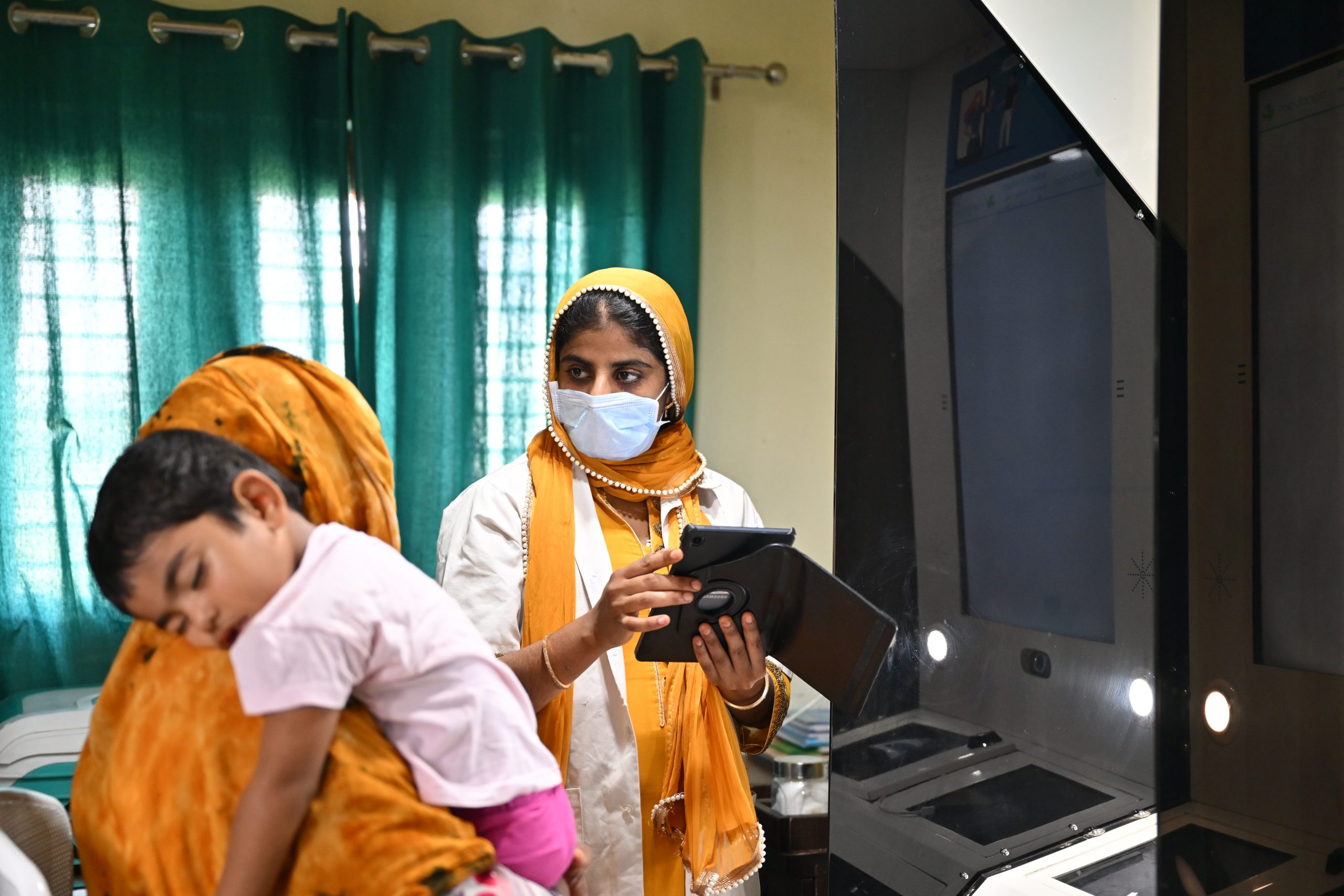
Health and Wellness Centres (HWCs)
In February 2018, the Government of India announced the establishment of 1,50,000 HWCs by transforming existing Sub-Centres and Primary Health Centres. These centres aim to deliver Comprehensive Primary Health Care (CPHC) and bring healthcare closer to people’s homes. HWCs are tasked with providing an expanded range of services, including maternal and child health, management of non-communicable diseases, early diagnosis of cancers, and referrals to specialised care. These centres also include provisions for free essential drugs and diagnostic services, ensuring accessible and affordable healthcare.
HWCs are designed to meet the primary healthcare needs of the population in their catchment area, focusing on principles of accessibility, universality, and equity. Health promotion and disease prevention form a central part of this initiative, engaging and empowering individuals and communities to adopt healthier lifestyles. The emphasis on preventive care aims to reduce the prevalence of chronic illnesses, thereby alleviating the burden on the overall healthcare system.

Pradhan Mantri Jan Arogya Yojana (PM-JAY)
PM-JAY, a key component of Ayushman Bharat, was launched on 23 September 2018 in Ranchi, Jharkhand, by Prime Minister Narendra Modi. It is the world’s largest health assurance scheme, providing a health cover of INR 5 lakh per family per year for secondary and tertiary care hospitalisation to over 12 crore poor and vulnerable families, amounting to approximately 55 crore beneficiaries.
PM-JAY replaced the earlier National Health Protection Scheme (NHPS) and subsumed the Rashtriya Swasthya Bima Yojana (RSBY), which was launched in 2008. In addition to families listed under the Socio-Economic Caste Census (SECC) 2011, it also covers families that were insured under RSBY but are not present in the SECC 2011 database.
The programme is fully funded by the Government of India, with the cost of implementation shared between the Central and State Governments. PM-JAY is designed to provide financial risk protection for vulnerable populations, ensuring they do not face catastrophic health expenditures.
Key Features of PM-JAY
The PM-JAY, touted as the world’s largest health assurance scheme, provides a cashless annual health cover of `5 lakh per family, benefiting over 55 crore Indians. From pre-existing conditions to post-hospitalisation care, the scheme covers an expansive range of treatments, ensuring no one is left behind.
Comprehensive Coverage: PM-JAY covers up to INR 5 lakh per family per year, applicable to secondary and tertiary hospitalisation across public and private hospitals.
Cashless and Paperless: Beneficiaries receive cashless access to healthcare services at the point of care, eliminating financial and administrative barriers.
Pre- and Post-Hospitalisation: The scheme includes expenses for up to three days of pre-hospitalisation and 15 days of post-hospitalisation, covering diagnostics, medicines, and follow-up care.
Pre-Existing Conditions: All pre-existing medical conditions are covered from day one, ensuring no exclusions.
No Restrictions: There are no restrictions on family size, age, or gender, providing equitable access to all eligible members.
Nationwide Portability: Beneficiaries can access services at any empanelled hospital across India, regardless of their state of residence.
Extensive Service List: The scheme encompasses approximately 1,929 medical procedures, including surgery, intensive care, diagnostics, medication, physician fees, room charges, and post-operative care.
Reimbursement for Public Hospitals: Public hospitals are reimbursed at par with private hospitals, fostering equity in healthcare delivery and incentivising improvements in public healthcare infrastructure.
Benefit Cover Under PM-JAY
The Pradhan Mantri Jan Arogya Yojana (PM-JAY) offers comprehensive health coverage aimed at addressing the challenges posed by earlier government-funded health insurance schemes, which had varying upper limits ranging from `30,000 to `3,00,000 annually per family. These limits led to fragmented healthcare access across states. PM-JAY, in contrast, provides cashless health insurance of up to `5,00,000 per family annually, covering secondary and tertiary care treatments.
Components Covered Under PM-JAY
The scheme ensures that all expenses incurred during the treatment process are included, such as:
Medical examination, treatment, and consultation
Pre-hospitalisation services
Medicines and medical consumables
Non-intensive and intensive care services
Diagnostic and laboratory investigations
Medical implant services where applicable
Accommodation benefits for hospitalisation
Food services for admitted patients
Complications during treatment
Post-hospitalisation follow-up care, extending up to 15 days
Family Floater Advantage
The INR 5,00,000 cover operates on a family floater basis, meaning the total amount can be utilised by any or all family members as needed. Unlike the earlier Rashtriya Swasthya Bima Yojana (RSBY), which imposed a cap of five family members, PM-JAY eliminates restrictions on family size and member age.
Pre-Existing Conditions
Another significant advantage of PM-JAY is the inclusion of pre-existing diseases from day one. Beneficiaries suffering from any medical condition prior to enrolment are eligible for treatment under the scheme immediately upon enrolment.
PM-JAY Benefits for Senior Citizens (70 Years and Above)
Senior citizens aged 70 and above are entitled to free medical treatment of up to INR 5 lakh per annum under PM-JAY.

Eligibility Criteria
The only criterion for eligibility is that the individual must be 70 years or older, verified through their Aadhaar card.
Benefits
Coverage for all pre-existing diseases from the first day of enrolment.
Access to treatment across more than 30,000 empanelled hospitals nationwide.
Obtaining the Ayushman Vay Vandana Card Senior citizens can easily acquire their Ayushman Vay Vandana Card through the Ayushman Bharat App, using their Aadhaar card for verification.

PMJAY and Timely initiation of Cancers
The scheme has also had a notable impact on cancer treatment in India. A study published in The Lancet Regional Health – Southeast Asia highlighted a 36 per cent improvement in the timely initiation of cancer treatment over the past six years, largely attributed to PM-JAY. Timely treatment initiation, defined as starting treatment within 30 days of diagnosis, saw significant gains, with most patients now beginning treatment within 20 days. The study compared outcomes for individuals diagnosed between 1995 and 2017 with those diagnosed after 2018, finding a marked improvement in timely treatment access post-PMJAY implementation. While timely treatment initiation increased by 30 per cent among non-enrolled individuals, the increase among PM-JAY beneficiaries was an impressive 90 per cent, reflecting the scheme’s effectiveness in reducing delays and ensuring critical care for underprivileged populations.
By bridging the gap in healthcare access, PM-JAY has empowered economically weaker sections to seek early and effective treatment, significantly improving health outcomes.
(The authors are Chair, Programme Advisory Committee, NIHFW; Director, Child Care Clinic, and Head, Apollo Hospitals, Noida.)

