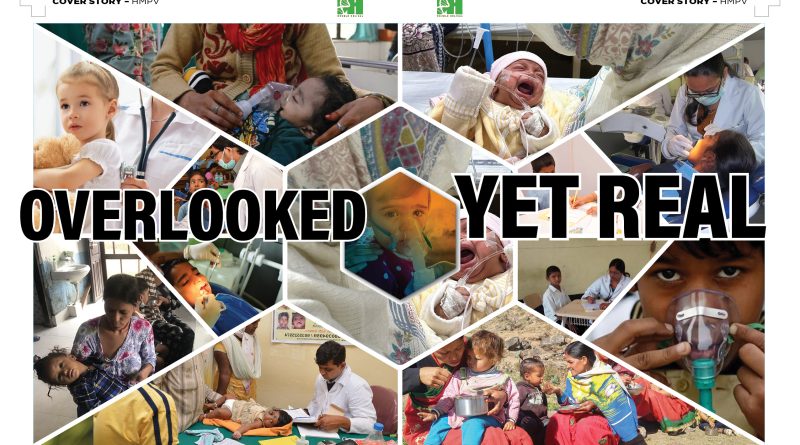
Overlooked Yet Real

Malnourished children are particularly vulnerable to viral infections, including HMPV, which are typically mild and self-limiting in well-nourished children. Malnutrition and child mortality in India, exacerbated by respiratory infections, presents a grim reality that often goes unnoticed by the media and policymakers.
By Dr Amitav Banerjee
In recent weeks, media outlets have been buzzing with alarming reports of widespread outbreaks of a respiratory virus, particularly among children, across many provinces in China. Hospitals in the country are reportedly overwhelmed with large numbers of cases, pushing health services to their limits. The virus responsible for these outbreaks has been identified as the Human Metapneumovirus (HMPV). Given the lingering trauma of the Covid-19 pandemic, such media reports about emerging viruses have reignited panic among the global population.
Is HMPV a New Virus?
Contrary to media speculation, HMPV is not a new virus. Although it was first identified in The Netherlands in 2001, HMPV has long been a part of the global virological landscape. This respiratory virus commonly infects children and is typically self-limiting. Sporadic reports of HMPV cases among children in India from various states align with what is well-documented in medical textbooks and should not cause undue alarm. Unfortunately, unnecessary media hype around what is essentially a garden-variety respiratory virus has amplified public anxiety. Serosurveys conducted on stored serum samples have revealed that HMPV has been circulating globally for over 50 years, underscoring its endemic nature.
Post-Pandemic Surges and the Concept of “Immunity Debt”

HMPV outbreaks in China are not an isolated phenomenon. Similar surges in respiratory viruses and other pathogens have been documented in various countries—including France, New Zealand, Australia, Italy, and the United Kingdom—in the post-pandemic period. These surges are particularly pronounced among children and can be attributed to a concept known as “immunity debt” or “immunity gap.”
Under normal circumstances, infants and children are routinely exposed to a variety of viruses and bacteria, which stimulate and prime their immune systems. However, during the Covid-19 pandemic, strict lockdown measures, along with other non-pharmaceutical interventions (NPIs) such as physical distancing, isolation, and the excessive use of sanitisers, significantly curtailed this natural process. As a result, large sections of the population—especially children—were left immune-naïve and vulnerable to common infections of childhood.
For instance, HMPV typically begins infecting children from six months of age. Under normal conditions, by the time they reach five years, 90-100 per cent of children would have encountered the virus, allowing their immune systems to develop appropriate defences. However, the harsh and prolonged restrictions in China, in place for nearly five years, disrupted this natural progression. Consequently, a large cohort of immune-naïve children is now encountering HMPV simultaneously, leading to widespread infections that would ordinarily have occurred gradually over time.

Assessing the Risks of HMPV
It is important to note that HMPV is a mild virus with low virulence. While it may lead to a high number of cases, it poses little risk of mortality in healthy children. Severe infections are primarily limited to immune-compromised individuals—whether children or the elderly—who are inherently vulnerable to a wide range of viral infections. For the general population, HMPV does not warrant special attention, provided that underlying co-morbidities are managed effectively.
Lessons for Future Pandemics
The phenomenon of immunity debt underscores an essential public health lesson: excessively strict restrictive measures, beyond a reasonable limit, may fail to achieve a net benefit for the population in the long term. Humans cannot live in sterile environments indefinitely. Once restrictions are lifted, the rebound in the transmission of common pathogens is inevitable, and the immunity debt must eventually be paid—often with interest. Infections can be postponed, but not permanently prevented.
Policymakers must weigh these trade-offs carefully when formulating responses to future pandemics. Public health strategies should strike a balance between protecting the population from immediate threats and preserving the natural processes that build immunity over time. Knee-jerk reactions and media-induced panic should give way to evidence-based approaches that prioritise long-term resilience over short-term containment.

The Burden of Child Malnutrition
Mild viruses such as HMPV and others typically cause mild, self-limiting infections in the majority of children. However, their impact can be devastating in immune-compromised individuals, particularly malnourished children. India, with one of the highest rates of child under-nutrition globally, faces an alarming public health crisis. Statistics reveal that 36 per cent of Indian children are stunted, reflecting lower height for age, 17 per cent are underweight, and 6 per cent suffer from severe malnutrition. These figures point to a widespread challenge with far-reaching implications.
This significant prevalence of under-nutrition compromises the immune systems of affected children, making them more vulnerable to viral infections, including HMPV, which would otherwise be mild and self-limiting in well-nourished children. Such encounters with pathogens set off a vicious cycle: malnourished children are more likely to suffer severe disease and even death. Those who survive these infections often emerge more malnourished than before, perpetuating the infection-malnutrition-infection cycle. This cycle remains a critical, yet under-addressed, factor in India’s child mortality statistics.
High Mortality Among Malnourished Children
India’s high child mortality rate, exacerbated by respiratory infections, paints a grim picture that often escapes the attention of media and policymakers. Approximately 400,000 deaths occur annually among children under the age of five due to respiratory infections—a stage of life when children are most likely to encounter HMPV. This staggering number translates to over 1,000 child deaths every day, many of whom belong to malnourished and marginalised communities. These deaths, occurring in the shadows of systemic neglect, fail to generate public or governmental concern.

If You Don’t Have Bread, Eat Cake!
It is a painful irony that mild infections, otherwise easily managed, are claiming the lives of so many children due to unresolved child malnutrition and inequitable access to healthcare services. Adding to this tragedy is the fact that costly diagnostic tests for HMPV are being offered by private laboratories to affluent sections of society, who are least likely to suffer from severe outcomes of such infections. Meanwhile, marginalised children, for whom such infections are often deadly, remain invisible to both media and policymakers.
Even more disconcerting is the clamour from certain quarters for increasing testing of a virus that is largely benign in healthy populations. This misplaced focus is reminiscent of the infamous remark attributed to Queen Marie-Antoinette during the French Revolution: “If you don’t have bread, eat cake.” It underscores the disconnect between public health priorities and the ground realities of underserved populations.

Addressing Silent Pandemics
India stands at a crossroads. To tackle child malnutrition effectively, the nation needs nothing short of a “Nutrition and Health Revolution.” The current allocation of resources towards widespread testing for relatively benign viruses is a misplaced priority. Instead, these funds must be redirected towards combating child malnutrition. Improving nutrition would bolster children’s immunity, enabling them to withstand a wide range of pathogens, rather than addressing infections on a case-by-case basis.
Equally critical is the urgent need to strengthen India’s public health infrastructure. Recent audits by the Comptroller and Auditor General (CAG) have exposed severe deficiencies in this domain. Many states face a 40-50 per cent shortfall in healthcare personnel, including doctors and paramedical staff, across government hospitals and health centres. These gaps directly impact the healthcare access of underprivileged populations, perpetuating health inequities.
As a nation, we must recognise that waiting for a hypothetical Disease ‘X’ pandemic is a luxury we cannot afford. Instead, the battle must begin now, targeting the root causes of our vulnerabilities. The real challenge lies in tackling the ‘silent pandemics’ of child malnutrition and unequal access to healthcare services. The path ahead is challenging, and the journey is long, but as the poet aptly said, “We have miles to go before we sleep.”.
(The author, a renowned epidemiologist and Professor Emeritus at DY Patil Medical College in Pune, has served in the armed forces for over two decades. Recently, he was ranked among the world’s top 2 per cent scientists by Stanford University.)