Targeted, Tailored, and Transformative
The treatment of gynaecological cancers has evolved remarkably, moving from radical surgeries to precision-driven, minimally invasive techniques. With advances in genomic profiling, targeted therapies, robotic surgery, immunotherapy and cutting-edge molecular diagnostics, the future of gynaecological cancer treatment is becoming increasingly personalised, offering reduced recovery time, improved patient outcomes, better survival and quality of life.
By Dr Pakhee Aggarwal

Over the years, the treatment of gynaecological cancers has seen remarkable advancements. From the early 1900s, when radical hysterectomy was introduced by Wertheim as a surgical procedure for cervical cancer, to today’s minimally invasive and targeted therapies, the landscape of cancer treatment has drastically evolved. These changes have significantly reduced surgical complications, improved patient recovery times, and enhanced overall treatment outcomes.
In recent years, breakthroughs in genomic profiling, molecular-based targeted therapies, precision radiation techniques, and cutting-edge chemotherapeutic advancements have paved the way for a more personalised approach to cancer treatment. With the emergence of immunotherapy and artificial intelligence-driven surgical techniques, the fight against gynaecological cancers has become more precise and effective than ever before.
Endometrial Cancer: Surgery and Beyond
Traditionally, surgery for endometrial cancer required a large incision through a midline laparotomy. This procedure involved removing the uterus, fallopian tubes, ovaries, and an extensive pelvic and para-aortic lymphadenectomy, along with peritoneal and omental biopsies. However, the advent of robotic-assisted surgeries has transformed this approach. Today, precision robotic surgery, coupled with sentinel lymph node mapping, has replaced open surgery, significantly reducing post-operative complications while maintaining the same cancer treatment effectiveness.
One of the key advantages of robotic surgery is its ability to offer a faster recovery, even in patients who have obesity, hypertension, or other comorbidities. The risk of developing lymphedema, a condition where excess fluid accumulates in tissues leading to swelling, is reduced by more than tenfold in robotic surgeries. As a result, patients can move on to the next stage of treatment—such as chemotherapy or radiation—much sooner than they would with traditional open surgery.
Additionally, augmented reality (AR) and artificial intelligence (AI) are being integrated into surgical techniques to further refine precision and improve patient outcomes.
From a molecular perspective, The Cancer Genome Atlas has classified endometrial cancer into four distinct types based on genetic mutations:
POLE mutated – Tumours with a good prognosis, often not requiring aggressive adjuvant treatment.
MMR deficient (MMRd) or microsatellite unstable (MSI-H) – A subtype that responds well to immunotherapy.
p53 mutated – Tumours with a poorer prognosis, requiring combined chemotherapy and radiotherapy.
Non-specific molecular profile (NSMP) – A category requiring further research for better treatment planning.
In advanced or recurrent cases, targeted therapies like PD-1/PD-L1 inhibitors (Pembrolizumab) and tyrosine kinase inhibitors (Lenvatinib) have revolutionised treatment by selectively attacking cancer cells while minimising damage to healthy tissues.
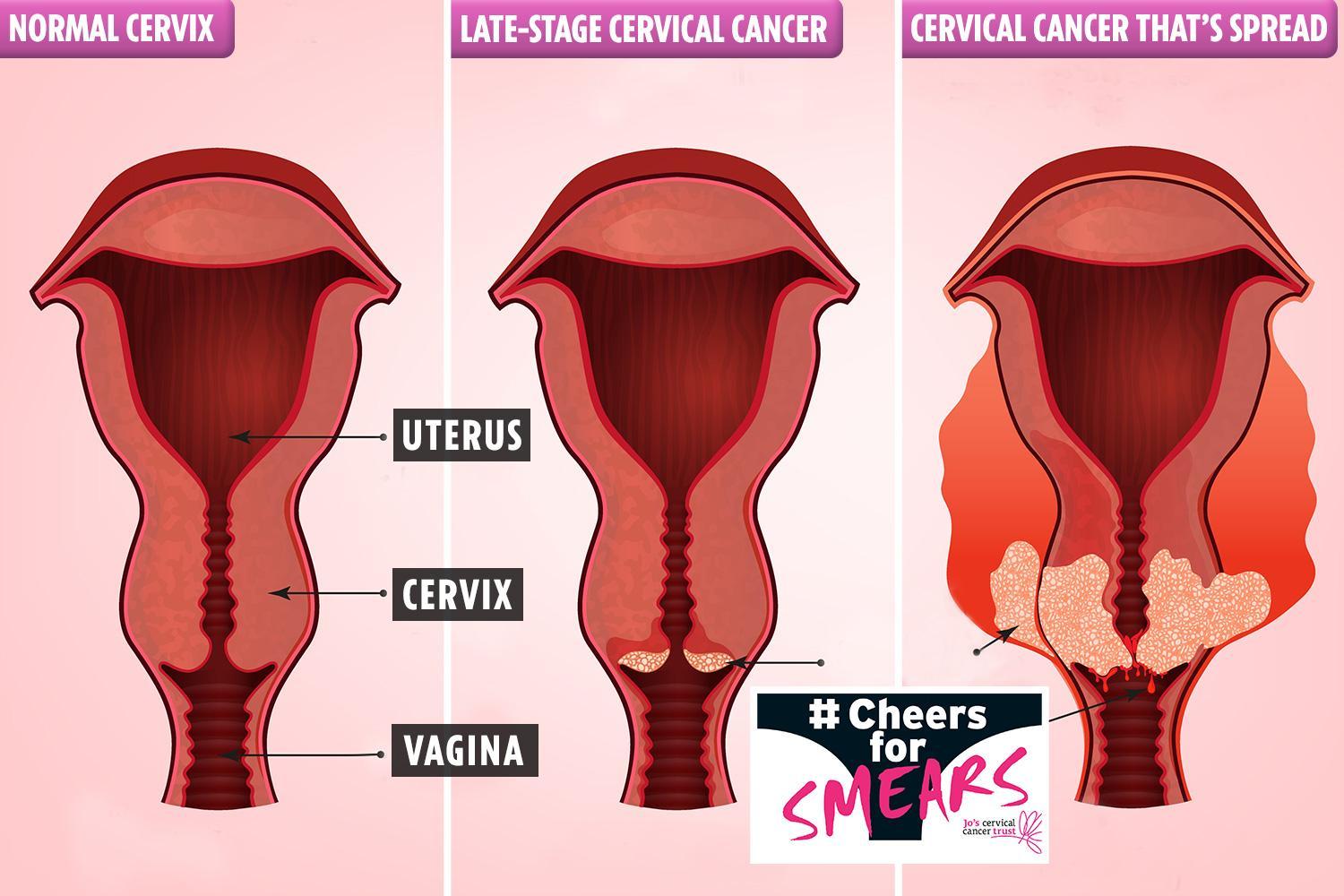
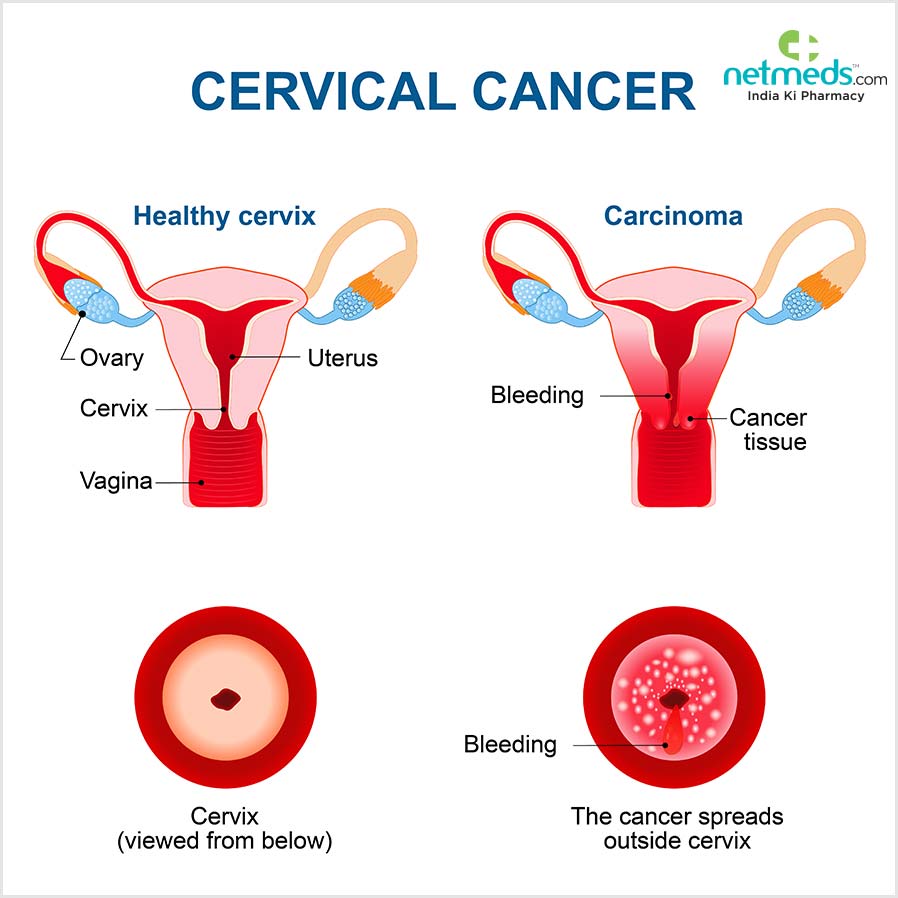
Cervical Cancer: Evolving Surgical and Radiation Therapies
Like endometrial cancer, cervical cancer treatment has evolved from traditional open surgery to minimally invasive approaches. One of the key advancements has been the introduction of nerve-sparing radical hysterectomy, which helps preserve bladder function. This means patients can have their urinary catheters removed sooner, leading to faster recovery and better post-surgical quality of life.
However, a major study called the LACC trial found that minimally invasive radical hysterectomy resulted in worse survival outcomes compared to open surgery. As a result, this technique has been put on hold. A counter-study, RACC trial, is currently underway to evaluate the feasibility of minimally invasive surgery for cervical cancer. For early-stage cervical cancer, sentinel lymph node mapping is gaining traction. Research has shown that for tumours smaller than 2 cm, simple hysterectomy is adequate, reducing surgical complications while maintaining effective cancer control (SHAPE trial).
Radiation therapy has also become more sophisticated, with Intensity-Modulated Radiotherapy (IMRT) and Image-Guided Radiotherapy (IGRT) delivering precise doses while minimising damage to surrounding organs. Meanwhile, in advanced cervical cancer, clinical trials like INTERLACE and KEYNOTE A018 are investigating the benefits of combining chemotherapy with immunotherapy for improved survival rates.

Ovarian Cancer: The Challenge of Late Diagnosis
Ovarian cancer is often diagnosed at an advanced stage (Stage III/IV), making treatment more complex. The standard treatment involves debulking surgery (removing as much tumour as possible), followed by six cycles of chemotherapy. In some cases, patients receive neoadjuvant chemotherapy before surgery to shrink the tumour, followed by interval debulking into the abdomen during surgery to enhance the treatment’s effectiveness. While the standard chemotherapy regimen includes platinum- and taxane-based drugs, advancements in anti-angiogenic therapy (which blocks the tumour’s blood supply)
Genetic and molecular profiling have further enhanced ovarian cancer treatment. Research shows that nearly 50% of high-grade serous ovarian cancers have a genetic mutation called Homologous Recombination Deficiency (HRD+), making them suitable candidates for PARP inhibitor (PARPi) therapy. These drugs, such as Olaparib, Niraparib, and Rucaparib, work by blocking an alternative DNA repair pathway, ultimately leading to cancer cell death. Another promising area of research involves Antibody-Drug Conjugates (ADCs), where cancer-specific antibodies are linked to a potent cytotoxic agent, delivering targeted therapy with minimal damage to healthy cells.
Vulvar Cancer: Advances in Surgery and Therapy
Surgical techniques for vulvar cancer have also improved significantly. Traditional radical vulvectomy, which required a large butterfly incision, has been replaced by a triple incision surgery or a wide local excision for smaller tumours. Sentinel lymph node mapping using technetium and indocyanine green (ICG) has helped minimise the need for extensive lymph node dissection, reducing complications.
For more complex cases, robotic surgery is being used for inguino-femoral lymph node excision, leading to better surgical precision and faster recovery. Reconstructive surgical techniques have also evolved, improving the quality of life for patients undergoing extensive tumour removal. Radiation therapy, chemotherapy, and immunotherapy have all contributed to preserving organ function while precisely targeting the tumour. Newer drug combinations are now available, ensuring better survival and post-treatment recovery.
The Future of Gynaecological Cancer Treatment
The latest trends indicate a clear shift towards personalised precision medicine, where treatment is tailored to a patient’s specific genetic profile, tumour type, and overall health condition. With continuous advancements in genomic research, targeted therapies, and minimally invasive techniques, cancer treatment is becoming more effective and less burdensome for patients. As research progresses, we can expect even more refined approaches that will further improve survival rates and quality of life for those diagnosed with gynaecological cancers.
(The author is Senior Consultant, Gynaecology Oncology & Robotic Surgery, Indraprastha Apollo Hospitals, New Delhi)

