Decibels of Destiny
The WHO warns that 2.5 billion people—one in four—will face hearing loss by 2050, costing nearly US$1 trillion annually. This invisible disability, long stigmatised and ignored, demands action to prevent, detect, and rehabilitate, with over 1 billion young adults at risk from unsafe listening. A modest US$1.40 per person could yield a 16-fold return, making ear care a global imperative.
By Dr Arun Agarwal/Dr Suneela Garg/Dr Arvind Garg/Dr Simantini Ghosh
On World Hearing Day 2025, the World Health Organization (WHO) invites the world to seize a transformative opportunity. This global campaign unites stakeholders, partners, and advocates in a shared mission that transcends mere commemoration—it’s a powerful call to action, urging individuals, communities, and governments to empower themselves and others to make ear and hearing care a universal reality. The urgency is undeniable: WHO projections paint a stark future where, by 2050, one in four people—nearly 2.5 billion individuals—will grapple with some degree of hearing loss, a significant rise from the one in five affected today. “Empower yourself to make ear and hearing care a reality for all!” the campaign declares, thrusting a long-neglected public health crisis into the foreground.
The Invisible Disability: A Stigmatised Crisis
“Hearing loss has often been referred to as an ‘invisible disability,’ not just because of the lack of visible symptoms, but because it has long been stigmatised in communities and ignored by policymakers,” asserts Dr Tedros Adhanom Ghebreyesus, WHO Director-General. This invisibility masks a pervasive challenge. Currently, over 5 per cent of the world’s population—equating to 430 million people, including 34 million children—requires rehabilitation to address their disabling hearing loss, defined as a loss greater than 35 decibels (dB) in the better hearing ear. Looking ahead to 2050, WHO forecasts that nearly 2.5 billion people will experience some form of hearing impairment, with over 700 million needing dedicated rehabilitative support. The economic toll is monumental: unaddressed hearing loss siphons nearly US$1 trillion annually from the global economy, a figure that accounts for health sector costs (excluding hearing devices), educational support expenses, lost productivity, and broader societal burdens.

The scale of this crisis is further illuminated by additional sobering statistics. Globally, over 80 per cent of ear and hearing care needs remain unmet, with nearly 80 per cent of individuals with disabling hearing loss living in low- and middle-income countries. The prevalence of hearing loss escalates with age—among those over 60, more than 25 per cent are affected by disabling hearing loss, a trend that underscores the growing burden on aging populations. Meanwhile, a younger demographic faces an equally pressing threat: over 1 billion young adults stand at risk of permanent, avoidable hearing damage due to unsafe listening practices, driven by the proliferation of personal listening devices (PLDs) and insufficient regulation of sound levels at entertainment venues. Yet, amidst this grim outlook, WHO offers a beacon of hope: scaling up ear and hearing care services worldwide requires an additional investment of just US$1.40 per person annually. Over a decade, this modest commitment promises a remarkable return of nearly US$16 for every dollar invested—a 16-fold yield in improved health outcomes, enhanced productivity, and elevated quality of life.
The Campaign’s Mission: Awareness and Action
World Hearing Day 2025 seeks to reframe ear and hearing health as a fundamental pillar of personal well-being and societal participation. The campaign’s multifaceted mission is to raise awareness about how to prevent deafness and hearing loss, promote ear care practices across the globe, and dismantle the pervasive stigma and policy neglect that Dr Tedros highlights. Deeply ingrained societal misperceptions and stigmatizing mindsets remain formidable obstacles, consistently thwarting efforts to address this escalating public health challenge and perpetuating its status as an overlooked epidemic.
Defining Hearing Loss and Deafness
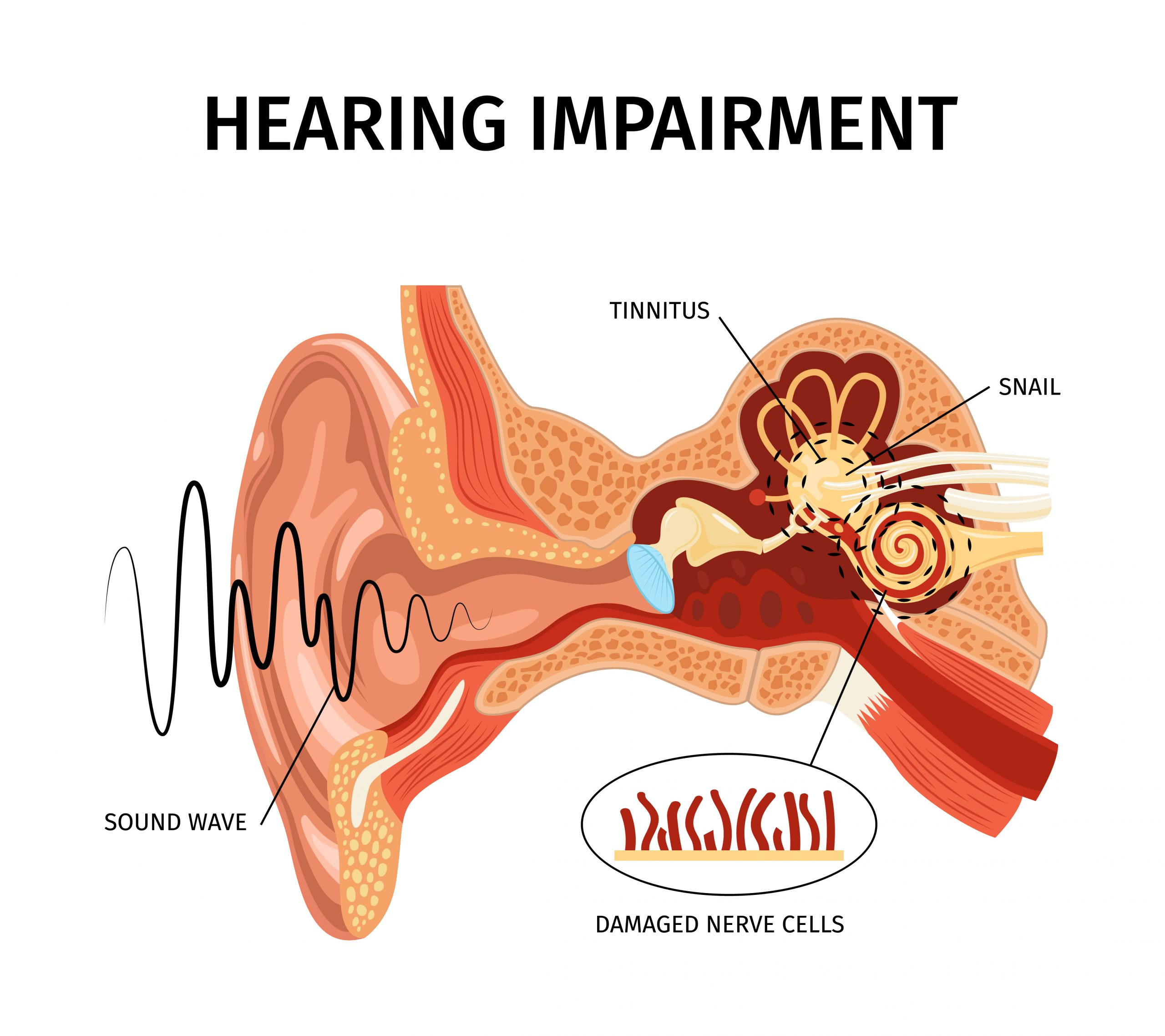
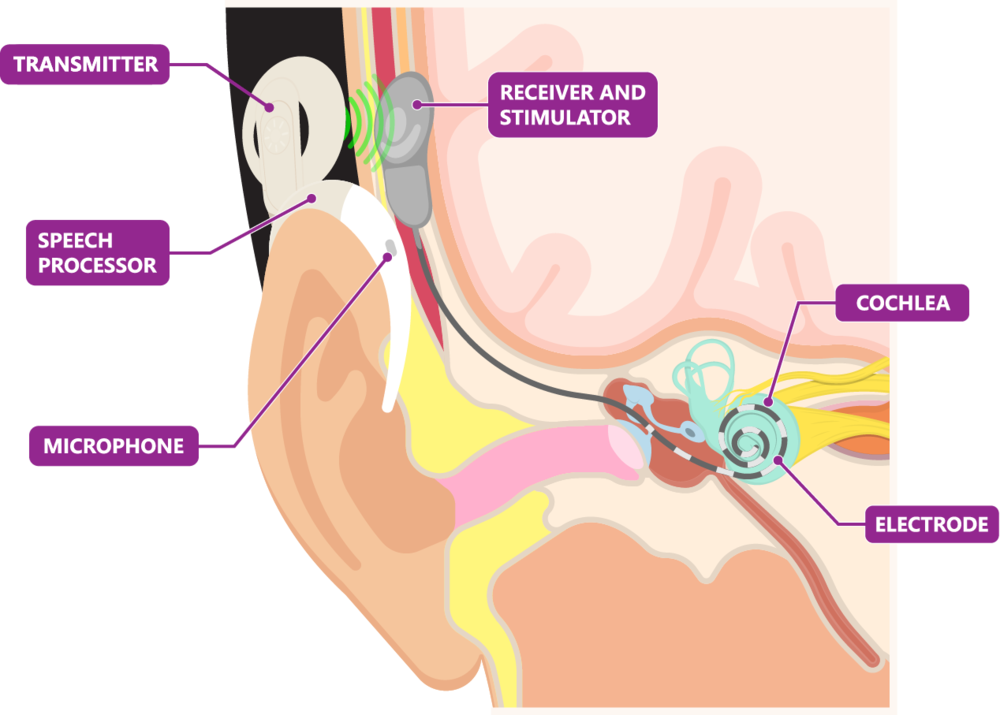
Hearing loss is clinically defined as occurring when an individual’s hearing thresholds exceed 20 dB in both ears—the established benchmark for normal hearing. This condition spans a broad spectrum: it can be mild, where soft sounds become difficult to discern; moderate; moderately severe; severe; or profound, where even loud sounds may be inaudible. Hearing loss can affect one ear (unilateral) or both (bilateral), disrupting the ability to perceive conversational speech or environmental sounds. Those classified as “hard of hearing” experience mild to severe loss and typically communicate through spoken language, often benefiting from hearing aids, cochlear implants, other assistive devices, and captioning services. In contrast, individuals who are “deaf” usually have profound hearing loss, implying little to no auditory perception; some utilize cochlear implants for partial restoration, while others rely on sign language as their primary mode of communication.
Causes Across the Life Span
The origins of hearing loss are diverse, striking at critical junctures across the human life span with varying degrees of susceptibility. During the prenatal period, genetic factors—both hereditary and non-hereditary—can lay the groundwork for hearing impairment, alongside intrauterine infections such as rubella and cytomegalovirus, which pose significant risks to foetal auditory development. The perinatal period introduces additional vulnerabilities, including birth asphyxia, where a lack of oxygen at birth can damage hearing structures; hyperbilirubinemia, marked by severe jaundice in newborns; low birth weight; and other perinatal morbidities, compounded by their medical management, which may inadvertently heighten risks.
In childhood and adolescence, chronic ear infections—specifically chronic suppurative otitis media—emerge as a leading cause, often accompanied by fluid buildup in the ear, known as chronic nonsuppurative otitis media. Infections like meningitis further threaten auditory health during these formative years. As individuals transition into adulthood and older age, the landscape shifts again: chronic diseases such as diabetes and hypertension, smoking, otosclerosis (abnormal bone growth in the ear), age-related sensorineural hearing loss, and sudden sensorineural hearing loss become prominent culprits. Across all ages, a host of factors can precipitate hearing loss, including cerumen impaction (impacted earwax), trauma to the ear or head, exposure to loud noises or sounds, ototoxic medicines like certain antibiotics and chemotherapy drugs, workplace exposure to ototoxic chemicals, nutritional deficiencies, viral infections, other ear conditions, and the delayed onset or progressive manifestation of genetic hearing loss.

The Profound Impact of Unaddressed Hearing Loss
When hearing loss goes unaddressed, its consequences reverberate across multiple dimensions of life, profoundly affecting individuals and societies alike. At the individual level, it imposes significant limitations on communication and speech, undermining the ability to connect with others. Cognition is adversely impacted, with studies linking hearing loss to accelerated cognitive decline. Socially, it fosters isolation, loneliness, and stigma—particularly among older adults, who may withdraw from social interactions due to frustration or embarrassment. These personal tolls ripple outward, exerting a substantial impact on society and the economy. Access to education and employment becomes restricted, with children in developing countries often excluded from schooling altogether due to a lack of accommodations. The WHO quantifies this burden, estimating an annual global cost of US$980 billion, which includes health sector expenses, costs of educational support, productivity losses, and societal impacts, measured in years lived with disability (YLDs) and disability-adjusted life years (DALYs). Tinnitus, a frequent companion to hearing loss, further compounds these challenges, eroding quality of life and exacerbating mental health struggles.
Prevention: A Lifeline Across the Life Course
Prevention offers a lifeline, and the good news is that much of this suffering can be averted. WHO estimates that nearly 60 per cent of childhood hearing loss arises from avoidable causes, which can be addressed through targeted public health strategies and clinical interventions implemented throughout the life course—from prenatal and perinatal stages to older age. In adults, the most common triggers, such as exposure to loud sounds and ototoxic medications, are similarly preventable with proactive measures. Effective strategies abound: immunisation programs against diseases like rubella and meningitis can safeguard hearing from infancy; robust maternal and childcare practices can mitigate perinatal risks like asphyxia and jaundice; genetic counseling can identify and manage hereditary predispositions early on; timely identification and treatment of common ear conditions, such as otitis media, can halt progression; occupational hearing conservation programs can protect workers from noise and chemical exposure; safe listening practices can curb recreational sound damage; and the rational use of medicines can prevent ototoxic hearing loss by prioritizing safer alternatives.

Identification and Management: Catching It Early
Early identification stands as the linchpin of effective hearing loss management, enabling interventions that can alter its trajectory. This requires systematic screening to detect hearing loss and related ear diseases among those most at risk, a group that spans newborns and infants, preschool and school-age children, individuals exposed to noise or chemicals in occupational settings, patients receiving ototoxic medications, and older adults. Hearing assessments and ear examinations can be conducted in both clinical and community settings, made increasingly accessible through innovative tools like the WHO’s hearWHO app and other technology-based solutions. These advancements allow screening with minimal training and resources, democratizing access to early detection. Once hearing loss is identified, addressing it as swiftly and appropriately as possible becomes essential to mitigate its adverse impacts, whether through technological aids, therapy, or environmental adjustments.
Rehabilitation: Empowering Independence
Rehabilitation serves as a cornerstone for empowering individuals with hearing loss to function at their optimum, enabling them to remain as independent as possible in everyday activities and to participate fully in education, work, recreation, and meaningful roles within their families and communities throughout their lives. This process encompasses a range of interventions tailored to individual needs: the provision of hearing technologies—such as hearing aids, cochlear implants, and middle ear implants—along with training in their use; speech and language therapy to enhance perceptive skills and develop communication and linguistic abilities; training in sign language and other sensory substitution methods, including speech reading, print-on-palm, Tadoma, and signed communication; the provision of hearing assistive technologies and services, such as frequency modulation (FM) and loop systems, alerting devices, telecommunication aids, captioning services, and sign language interpretation; and counselling, training, and support to boost engagement in education, employment, and community life. Comorbid conditions like cognitive impairment and tinnitus, which often accompany hearing loss, further highlight the need for a holistic approach, as these conditions significantly impact health and well-being, often leading to poorer quality of life.

The Noise Crisis: Unsafe Listening Practices
Unsafe listening practices—defined as listening to music or audio content at high volumes or for prolonged periods—pose a growing threat, particularly among adolescents and young adults worldwide. This trend is fuelled by the widespread availability of PLDs and the scarce enforcement of regulatory measures for both personal devices and entertainment venues. The risk of hearing loss hinges on three factors: the loudness, duration, and frequency of noise exposure. Permissible levels of recreational noise exposure are often calculated from equivalent occupational noise limits, such as 80 dB for 40 hours per week or 85 dB for 40 hours per week, though these standards vary slightly by region and regulatory body. Sound intensity, measured on a logarithmic scale, involves a time-intensity trade-off (exchange rate): for example, based on a maximum permissible level of 80 dB for 8 hours a day (40 hours/week) with a 3 dB exchange rate, permissible exposure drops to 2.5 hours at 92 dB, 38 minutes at 98 dB, and just 19 minutes at 101 dB. PLD users frequently choose volumes as high as 105 dB, while average sound levels at entertainment venues range from 104 to 112 dB, exceeding safe limits even for brief durations. These findings suggest that many young people are at risk of permanent hearing loss. While systematic reviews have explored unsafe listening practices, estimates of their prevalence and global burden remain absent from published literature, a gap that hinders prevention efforts and the ability to effectively communicate the need for intervention to governments, industries, and stakeholders responsible for policy implementation.
WHO’s Safe Listening Initiatives
WHO estimates that over 1 billion young people globally are at risk of hearing loss due to sound exposure in recreational settings—a preventable yet costly threat. In response, governments, public health agencies, music creators, distributors, amplifiers, the private sector, civil society, and other stakeholders bear a duty of care to understand sound levels and foster safe listening environments. The Make Listening Safe initiative has birthed two landmark standards to address this crisis. The Global Standard for Safe Listening Venues and Events comprises six features designed to protect hearing while preserving artistic integrity: an upper sound level limit of 100 dB LAeq (15-minute average) ensures safety and enjoyment; live sound level monitoring by designated staff using calibrated equipment tracks exposure in real time; optimised venue acoustics and sound systems enhance quality while minimizing harm; personal hearing protection, such as earplugs with instructions, is made available to audience members; designated quiet zones allow attendees to rest their ears, reducing damage risk; and appropriate training and information ensure that both staff and audiences understand practical steps for safe listening. These recommendations can be implemented by governments through legislation, compliance monitoring, and public awareness campaigns—recognizing that hearing loss prevention improves quality of life and yields productivity gains—by venue owners and managers who can voluntarily adopt features to protect patrons and enhance their experience, and by acousticians, engineers, musicians, and event organizers who can integrate the standard’s benefits into their training and practice, safeguarding both audiences and workers.
The WHO-ITU Global Standard for Personal Audio Systems and Devices equips PLDs with safe listening features: a dosimetry function includes software that tracks sound exposure as a percentage of a reference “sound allowance,” offering users two modes—80 dB for 40 hours per week for adults and 75 dB for 40 hours per week for children—to determine their safe sound dose; personalised information generates an individualised listening profile based on user habits, informing them of safety levels and providing action cues; volume limiting options include automatic reduction based on profile data (lowering volume if it’s too high for too long) and password-protected parental controls to set safe levels for children; and general information provides guidance on safe listening practices across personal devices and leisure activities, alongside risks of non-compliance.
India’s Hearing Landscape: NPPCD Data
In India, the National Programme for Prevention and Control of Deafness (NPPCD) offers a detailed snapshot of the hearing loss burden: unilateral hearing loss (≥25 dB) affects 2.8 per cent of the population; bilateral hearing loss (≥25 dB in the better ear) impacts 7.1 per cent; total hearing loss or ear disability stands at 9.9 per cent, with a notable disparity between urban areas (8.6 per cent) and rural areas (11.2 per cent, p<0.01); and disabling hearing loss (DHL) affects 2.9 per cent, again higher in rural settings (3.4 per cent) than urban (2.3 per cent, p<0.01). DHL is defined as greater than 30 dB in the worse ear for those under 15 years and greater than 40 dB for those 15 and older, highlighting age-specific thresholds.
Implications and Barriers
The implications of unaddressed hearing loss are vast, disrupting listening and communication, language and speech development, cognition, education, employment, and financial well-being. It fosters social isolation, loneliness, and challenges to mental health, interpersonal relationships, identity, and stigma. Barriers to progress are equally formidable: a pervasive lack of awareness about ear care leaves many uninformed; teachers often lack the skills to identify children with hearing loss, delaying intervention; myths and misconceptions, alongside gender disparities, health system deficiencies, and policy-level inertia, further obstruct solutions.
A Vision for the Future
World Hearing Day 2025 reaffirms that hearing health across the life course is attainable. By preventing avoidable loss, detecting it early, and rehabilitating those affected, we can bridge the 80 per cent gap in unmet care needs. The campaign’s clarion call—to recognize hearing health as integral to a full life—demands collective action. With a modest investment, the world can mute the trillion-dollar toll of hearing loss, ensuring that silence no longer defines anyone’s existence.