Mind Your Brain
Tumours of the brain may not all be cancerous; there are benign tumours too. There are many typed of brain tumour and the symptoms vary. What causes a brain tumour? And what is the best treatment? Read on to know more
By Team Double Helical
Persistent symptoms like headaches that gradually become more frequent and severe, unexplained nausea or vomiting, vision problems like blurred vision, double vision or loss of peripheral vision, gradual loss of sensation or movement in an arm or a leg, difficulty with balance, speech difficulties and confusion in everyday matters are all possible symptoms of a brain tumour.
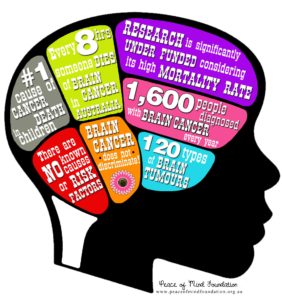
Early symptoms can be subtle or obvious, depending on the type, size, and location of the tumour. However, these problems do not necessarily point to the presence of a brain tumour either. No one knows what causes brain tumours; there are only a few known risk factors that have been established by research.
Children who are exposed to radiation to the head have a higher risk of developing a brain tumour in adulthood, as do people who have certain rare genetic conditions such as neurofibromatosis or Li-Fraumeni syndrome. But such cases represent a fraction of the approximately 35,000 new primary brain tumours diagnosed each year. Age is also a determinant; people over the age of 65 are diagnosed with brain cancer at a rate four times higher than younger people.
Although all such growths are generically called brain tumours, not all brain tumours are cancerous. Cancer is a term reserved for malignant tumours. Malignant tumours can grow and spread aggressively, overpowering healthy cells by taking their space, blood, and nutrients. They can also spread to distant parts of the body.
Now-a-days, neuro-navigation systems enable surgeons to visualize the anatomy of a patient’s brain during surgery and precisely track the location of their surgical instruments in relation to the anatomy, even accommodating for the brain shift that occurs during surgery. Using StealthStation technologies during procedures like tumour resections, surgeons can navigate more precisely, perform less-invasive procedures, and help improve clinical outcomes
If a brain tumour is diagnosed, providing relief from symptoms remains an important part of a patient’s care and treatment. Today, most tumours can be removed safely with microsurgical techniques in a manner that maximizes tumour removal and minimizes harm to the patients. How quickly a brain tumour grows can vary greatly. The growth rate as well as location of a brain tumour determines how it will affect the function of a patient’s nervous system. Brain tumour treatment options depend on the type of brain tumour the patient has as well as its size and location.
A brain tumour is a mass or growth of abnormal cells in a person’s brain or anywhere close to the brain. Brain tumours may begin in the brain (primary brain tumours), or cancer in other parts of the body may spread to the brain (secondary, or metastatic, brain tumours). There are many different types of brain tumours; while some brain tumours are noncancerous (which are called benign); some are cancerous (which are called malignant).
Signs and Symptoms
The signs and symptoms of a brain tumour vary greatly and depend on the brain tumour’s size, location and rate of growth. General signs and symptoms may include onset of or change in pattern of headache, headaches that gradually become more frequent and more severe, unexplained nausea or vomiting, vision problems, such as blurred vision, double vision or loss of peripheral vision, gradual loss of sensation in or movement of an arm or a leg, difficulty with balance, speech difficulties, confusion in everyday matters, personality or behavioural changes, seizures, especially in someone who doesn’t have a history of seizures and hearing problems.
There are many types of primary brain tumours each with a nomenclature according to the type of cells involved. Among them, gliomas begin in the brain or spinal cord and include astrocytomas, ependymoma, glioblastomas, oligoastrocytomas and oligodendrogliomas. Meningiomas are tumours that arise from the membranes that surround the brain and spinal cord (meninges). Most meningiomas are non-cancerous. Acoustic neuromas (schwannomas) are benign tumours that develop on the nerves that control balance and hearing leading from the inner ear to the brain. Then, the pituitary adenomas are tumours that are mostly benign which develop in the pituitary gland at the base of the brain. These tumours can affect the pituitary hormones affecting the entire body. The most common cancerous brain tumours in children are the medulloblastomas that start in the lower back part of the brain and tend to spread through the spinal fluid. These tumours are less common, though they do occur, in adults.
Primitive neuro-ectodermal tumours (PNETs) are rare, cancerous tumours that start in embryonic (foetal) cells in the brain. They can occur anywhere in the brain. Germ cell tumours are those that may develop during childhood where the testicles or ovaries would be formed. But sometimes germ cell tumours move to other parts of the body, such as the brain. Craniopharyngiomas are the rare, noncancerous tumours that start near the brain’s pituitary gland, which secretes hormones that control a number of body functions. As the craniopharyngioma slowly grows, it can affect the pituitary gland and other structures near the brain.
Secondary (metastatic) brain tumours are tumours that result from cancer that starts elsewhere in the body and then spreads to the brain. Secondary brain tumours most often occur in people who have a history of cancer. But in rare cases, a metastatic brain tumour may be the first sign of cancer that began elsewhere in the body. Secondary brain tumours are far more common than primary brain tumours. Any cancer can spread to the brain, but the most common types include breast cancer, colon cancer, kidney cancer, lung cancer and melanoma.
In most people with primary brain tumours, the cause of the tumour is not clear. But doctors have identified some factors that may increase the risk of brain tumour. The risk of a brain tumour increases as one ages. Brain tumours are most common in older adults. However, a brain tumour can occur at any age. And certain types of brain tumours occur almost exclusively in children. People who have been exposed to a type of radiation called ionizing radiation have an increased risk of brain tumour. Ionizing radiation includes that from radiation therapy used to treat cancer and radiation exposure caused by atomic bombs.
More common forms of radiation, such as electromagnetic fields from power lines and radiofrequency radiation from cell phones and microwave ovens have not been proved to be linked to brain tumours.
A small percentage of brain tumours occurs in people with a family history of brain tumours or a family history of genetic syndromes that increase the risk of brain tumours. If it is suspected that a patient may have a brain tumour, the doctor may recommend a number of tests and procedures. Magnetic resonance imaging (MRI) is commonly used to help diagnose brain tumours. In some cases, a dye may be injected through a vein in the arm during the MRI study called MRI with contrast. Other imaging tests may include computerised tomography (CT) scan and positron emission tomography (PET).
If it is suspected that the brain tumour may be a result of cancer that has spread from another area of the body, the doctor may recommend tests and procedures to determine where the cancer originated. For example, a CT scan of the chest may be conducted to look for signs of lung cancer. A biopsy may be performed as part of an operation to remove the brain tumour, or a biopsy can be performed using a needle. The biopsy sample is then viewed under a microscope to determine if it is cancerous or benign. This information is critical to establish a diagnosis and prognosis and, most importantly, in guiding treatment.
 Treatment
Treatment
Treatment for a brain tumour depends on the type, size and location of the tumour.
Surgery
If the brain tumour is located in a place that makes it accessible for an operation, the neuro- surgeon will work to remove as much of the brain tumour as possible. In some cases, tumours are small and easy to separate from surrounding brain tissue, which makes complete surgical removal possible. In other cases, tumours cannot be separated from surrounding tissue or they may be located near sensitive areas in the brain, making surgery risky. In these situations only a part of the tumour is removed which is safe.
Removing a portion of the brain tumour may help reduce the signs and symptoms. Surgery to remove a brain tumour carries risks such as infection and bleeding. Other risks may depend on the part of the brain where the tumour is located. For instance, surgery on a tumour near nerves that connect to the eyes may carry a risk of vision loss.
Radiation therapy
Radiation therapy uses high-energy beams, such as X-rays or protons to kill tumour cells. Radiation may emanate from a machine outside a patient’s body (external beam radiation), or, in very rare cases, it may be from inside the body close to the brain tumour (brachytherapy).
External beam radiation can focus just on the area of the brain where the tumour is located, or it can be applied to the entire brain (whole-brain radiation). Whole-brain radiation is most often used to treat cancer that has spread to the brain from some other part of the body. Side effects of radiation therapy depend on the type and dose of radiation a patient receives. Common side effects during or immediately following radiation include fatigue, headaches and scalp irritation.
Radio surgery
In stereotactic radio surgery multiple beams of radiation give a highly focused form of radiation treatment to kill the tumour cells in a very small area. Each beam of radiation is not particularly powerful, but the point where all the beams meet — at the brain tumour — receives a very large dose of radiation to kill the tumour cells.
There are different types of technology used in radio surgery to deliver radiation to treat brain tumours, such as a Gamma Knife, available in cancer institutions. Radio surgery is typically done in one session, and in most cases the patient can go home the same day.
Chemotherapy
Chemotherapy uses drugs to kill tumour cells. The drugs can be taken orally in a pill form or injected into a vein (intravenously). The side effects depend on the type and dose of drugs administered. It can cause nausea, vomiting and hair loss.
Targeted drug therapy
Targeted drug treatments focus on specific abnormalities present within cancer cells.
Rehabilitation after treatment
Since brain tumours can develop in parts of the brain that control motor skills, speech, vision and thinking, rehabilitation may be a necessary part of recovery. Doctors may refer patients to particular services that would be of help.
Physical therapy can help one regain lost motor skills or muscle strength. Occupational therapy can help a patient get back to normal daily activities, including work, after a brain tumour or other illness. Speech therapy with the help of speech pathologists can help in the event of difficulty in speaking.