Exclusive: National Medical Commission Bill Fight For Right
The much talked National Medical Commission Bill provides for the constitution of four autonomous boards entrusted with conducting undergraduate and postgraduate education, accreditation of medical institutions and registration of practitioners under the National Medical Commission. But with was any improvement perceived? None to the eyes of many and that was the reason it was not continued with. Replacing one body with another will not serve any purpose unless doctors faternity do a brainstorming about the underlying reasons as to why even the Government appointed Board could not redeem the image of Medical Council of India…
By Amresh Kumar Tiwary
An aim to repeal the Indian Medical Council Act, 1956 and provide for a medical education system which ensures like availability of adequate and high quality medical professionals, adoption of the latest medical research by medical professionals, periodic assessment of medical institutions, and an effective grievance redressal mechanism, the Minister of Health and Family Welfare, Govt of India has already introduced the National Medical Commission(NMC) Bill, 2017 in Lok Sabha on December 29, 2017.
But Indian Medical Association (IMA) has strongly opposed the draft bill that seeks to replace the Medical Council of India with a new body, claiming it will cripple the medical profession. IMA appealed to the Prime Minister to revise the draft bill in the larger interest of the medical profession.
Key features of the Bill include Constitution of the National Medical Commission: The Bill sets up the National Medical Commission (NMC). Within three years of the passage of the Bill, state governments will establish State Medical Councils at the state level. The NMC will consist of 25 members, appointed by the central government. A Search Committee will recommend names to the central government for the post of Chairperson, and the part time members. These posts will have a maximum term of four years. The Search Committee will consist of seven members including the Cabinet Secretary and three experts nominated by the central government (of which two will have experience in the medical field).
Members of the NMC will include: (i) the Chairperson, (ii) the President of the Under-Graduate Medical Education Board, (iii) the President of the Post-Graduate Medical Education Board, (iv) the Director General of Health Services, Directorate General of Health Services, (v) the Director General, Indian Council of Medical Research, and (vi) five members (part-time) to be elected by the registered medical practitioners from amongst themselves from the prescribed regional constituencies under the Bill.
Functions of the National Medical Commission: Functions of the NMC include: (i) framing policies for regulating medical institutions and medical professionals, (ii) assessing the requirements of healthcare related human resources and infrastructure, (iii) ensuring compliance by the State Medical Councils of the regulations made under the Bill, (iv) framing guidelines for determination of fees for up to 40% of the seats in the private medical institutions and deemed universities which are regulated as per the Bill.
Medical Advisory Council: Under the Bill, the central government will constitute a Medical Advisory Council. The Council will be the primary platform through which the states/union territories can put forth their views and concerns before the NMC. Further, the Council will advise the NMC on measures to enable equitable access to medical education.
Autonomous boards: The Bill sets up certain autonomous boards under the supervision of the NMC. Each autonomous board will consist of a President and two members, appointed by the central government. These boards are: (i) the Under-Graduate Medical Education Board (UGMEB) and the Post-Graduate Medical Education Board (PGMEB): These Boards will be responsible for formulating standards, curriculum, guidelines, and granting recognition to medical qualifications at the undergraduate and post graduate levels respectively, (ii) the Medical Assessment and Rating Board (MARB):
The MARB will have the power to levy monetary penalties on medical institutions which fail to maintain the minimum standards as laid down by the UGMEB and the PGMEB. The MARB will also grant permission for establishing a new medical college, and (iii) the Ethics and Medical Registration Board: This Board will maintain a National Register of all licensed medical practitioners, and regulate professional conduct. Only those included in the Register will be allowed to practice medicine.
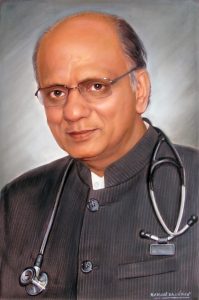
 Dr Shishir Narayan, Shroff Eye Hospital, New Delhi, said, “There will be a uniform National Eligibility-cum-Entrance Test for admission to under-graduate medical education in all medical institutions regulated by the Bill. The NMC will specify the manner of conducting common counselling for admission in all such medical institutions”.
Dr Shishir Narayan, Shroff Eye Hospital, New Delhi, said, “There will be a uniform National Eligibility-cum-Entrance Test for admission to under-graduate medical education in all medical institutions regulated by the Bill. The NMC will specify the manner of conducting common counselling for admission in all such medical institutions”.
“There will be a National Licentiate Examination for the students graduating from medical institutions to obtain the license for practice. The National Licentiate Examination will also serve as the basis for admission into post-graduate courses at medical institutions”, he added.
The draft National Medical Commission Bill provides for the constitution of four autonomous boards entrusted with conducting undergraduate and postgraduate education, accreditation of medical institutions and registration of practitioners under the National Medical Commission.
According to Ravi Wankhede, National President, IMA, the NMC will “cripple” the functioning of the medical profession by making it completely answerable to the bureaucracy and non-medical administrators.
Regulators need to have autonomy and be independent of the administrators. The National Medical Commission will be a regulator appointed by the administrators under their direct control.
It abolishes the Medical Council of India and “possibly” Section 15 of the IMC Act, which says that the basic qualification to practice modern medicine is MBBS.
It takes away the voting right of every doctor in India to elect their medical council. The Medical Council of India is a representative body of the medical profession in India. Any registered medical practitioner in the country can contest the election and every qualified doctor can vote. Abolishing a democratic institution and replacing it by a body in which majority are nominated by the government is certainly a retrograde step.
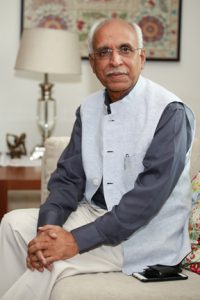
Dr. Ravi Wankhedkar, National President, IMA, said, “The draft bill, in its current form allows the private medical colleges to charge at will, nullifying whatever solace the NEET brought. The government can fix the fee for only 40% of the seats in private medical colleges. Also, it inducts non-medical people into the highest body of medical governance changing its perspective and character forever and introduces schedule IV to allow the AYUSH graduates to get registration in modern medicine.”
Dr K K Aggarwal, Ex National President, said, “We already appeal to our Prime Minister Narendra Modi to recall the bill and rectify these anomalies. Parliament has a larger role to protect the interest of the medical profession of the country.”
According to the draft bill, the commission will have government-nominated chairman and members, and the board members will be selected by a search committee under the Cabinet Secretary. There will five elected and 12 ex-officio members in the commission.
The draft bill also proposes a common entrance exam and licentiate exam which all medical graduates will have to clear to get practising licences. As per the provisions of the draft bill, no permission would be needed to add new seats or to start post-graduate courses.
National Medical Commission Bill 2017 sparks pan-India strike by doctors
Doctors in India recently went on a nationwide strike to protest against the draft National Medical Commission (NMC) Bill 2017. Indian Medical Association (IMA) has strongly opposed the bill.
The NMC bill seeks to replace the apex medical education regulator, the Medical Council of India (MCI), with a new body National Medical Commission (NMC). It is against this bill that doctors have decided to go on strike, leaving the fate of patients requiring urgent treatment hanging in the balance. Around 2.9 lakh doctors have come onto the streets in protest.
Here is what National Medical Commission (NMC) Bill is:
1) The bill seeks to replace the Medical Council of India with National Medical Commission as top regulator of medical education in India.
2) The bill also seeks to put in place a common entrance exam and licentiate exam, which all medical graduates will have to clear to get practicing licenses.
3) It would also put in place a four-tier structure for the regulation of medical education. The 20 members National Medical Commission will be at the top of this structure.
4) NMC will be a 20 member body comprising a Chairperson, a member secretary, eight ex-officio members and 10 part-time members.
5) Out of the 8 ex-officio members, four shall be presidents of the boards constituted under the act and remaining four shall be nominees from three ministries viz. Health, Pharmaceuticals, HRD and one from Director General of Health Services.
6) The bill also has a provision for a common entrance exam and licentiate (exit) exam that medical graduates have to pass before practicing or pursuing PG courses. For MBBS, students have to clear NEET, and before they step into practice, they must pass the exit exam.
7) The NMC can permit a medical professional to perform surgery or practice medicine without qualifying the National Licentiate Examination, in circumstances that may be specified in regulations.
8) According to the NMC Bill, the Ethics and Medical Registration Board can maintain a separate national register that would have the names of licensed AYUSH practitioners. The names of graduates of Bachelor of Ayurvedic Medicine and Surgery and Bachelor of Homeopathic Medicine and Surgery are already registered with their respective councils and on taking the bridge course they would be incorporated in a separate register maintained by the NMC, resulting in dual registration with two councils, which is neither open nor permissible.
9) The government, under the National Medical Commission (NMC), can dictate guidelines for fees up to 40% of seats in private medical colleges. This is aimed at giving students relief from the exorbitant fees charged by these colleges and is a standout feature of the bill.
Suggestions of IMA on National Medical Commission Bill, 2017
-Bill number 279 of 2017, introduced in lower house(Lok Sabha), The National Medical Commission Bill
-Ninety Second report of department related Parliamentary Standing Committee on Health and Family Welfare
-Ranjit Roy Chaudhary Expert Committee report submitted in February 2015.
-Opinion of IMA submitted to NITI Ayog on NMC
 According to A K Agarwal, Professor of Excelence and Medical Advisor, Apollo Group of Hospitals, the Parliamentary Standing Committee, in its report submitted to the Parliament on 8th March 2015 had highlighted the challenges faced by the health sector in India. The most important concerns of the Committee were large gaps in health care and universal health care goals, shortage of qualified doctors, specialists, super specialists, geographical mal-distribution of medical colleges, disconnect between medical education system and health care system and inadequate in self regulatory process.
According to A K Agarwal, Professor of Excelence and Medical Advisor, Apollo Group of Hospitals, the Parliamentary Standing Committee, in its report submitted to the Parliament on 8th March 2015 had highlighted the challenges faced by the health sector in India. The most important concerns of the Committee were large gaps in health care and universal health care goals, shortage of qualified doctors, specialists, super specialists, geographical mal-distribution of medical colleges, disconnect between medical education system and health care system and inadequate in self regulatory process.
Prof. Ranjit Roy Chaudhary Committee constituted in 2014 by Government of India submitted its report and suggested a new regulatory structure for modern medicine.
 Dr. Ravi Wankhedkar National President, IMA, said, “We are concerned to note that most of the recommendations of the Parliamentary Standing Committee or Prof. Ranjit Roy Chaudhary Committee do not find a place in the NMC Bill. On the other hand NMC Bill contains many clauses that are not as per the recommendation of the above committee. There are also contradictions between the objectives of the Bill and the clauses there under, eg. The Parliamentary Standing Committee did not mention about separate registration for AYUSH with bridge course which is included in the NMC Bill. Fixing fees is not within in the purview and powers of NMC.”
Dr. Ravi Wankhedkar National President, IMA, said, “We are concerned to note that most of the recommendations of the Parliamentary Standing Committee or Prof. Ranjit Roy Chaudhary Committee do not find a place in the NMC Bill. On the other hand NMC Bill contains many clauses that are not as per the recommendation of the above committee. There are also contradictions between the objectives of the Bill and the clauses there under, eg. The Parliamentary Standing Committee did not mention about separate registration for AYUSH with bridge course which is included in the NMC Bill. Fixing fees is not within in the purview and powers of NMC.”
Basically the objectives of the NMC Bill is to provide for a medical education system that ensures availability of adequate and high quality professionals that encourages medical professionals to adopt latest medical research work and to contribute to research.
The various clauses in NMC Bill, like single inspections of medical college, provision for increasing the seats of under graduates, freedom to start PG courses without inspection and increase the seats at the discretion of the medical colleges will definitely dilute the maintenance of the highest standards of medical educations and against the objective of NMC.
Section 31(8) of the NMC Bill is also contradictory to the definition of modern medicine. Section 31(8 EMR Board shall maintain a separate National Register including the names of licensed Ayush Practitioners who qualifies the bridge course referred in Section 49(4) in such manner as may be specialized by Regulators. By an explanation, Ayush it has been defined as a person who is a practitioner of Homeopathy or a practitioner of Indian Medicine as defined in clause(e) of Subsection 1 of the section 2 of the Indian Medicine Central Council Act, 1970 and is contradictory to the definition of Modern Medicine.
Ayush Bridge Course
The Parliamentary Standing Committee on health has never mentioned Ayush Bridge Course NMC in its chapter V clause 49(3),(4): clause 54(O) has suggested Ayush Bridge Course and separate National register for practioners who qualify the bridge course. It has to be noted that the systems are naturally contradictory and non complimentary.
National Medical Commission is a regulatory body for modern medical practitioners. It can contain only one type of registration that is those who have passed MBBS. Having a separate register for Ayush practitioners with bridge course to practice modern medicine amounts to legalisation of quackery.
 Dr Mangesh Pate, Joint Secrtary, IMA New Delhi, said, “We demand the deletion of separate register for AYUSH. Ethics and Medical Registration Board shall contain only one register that too only for MBBS.
Dr Mangesh Pate, Joint Secrtary, IMA New Delhi, said, “We demand the deletion of separate register for AYUSH. Ethics and Medical Registration Board shall contain only one register that too only for MBBS.
To solve the issue of non availability of doctors in PHC after internship one year compulsory posting in rural area to be mandatory or special packages to attract MBBS doctors should be provided.
The PHC’s are to be classified as very difficult rural area, difficult rural area and rural area. For very difficult and difficult rural area a special package should be made to attract MBBS doctors. Those who opt for these PHC’s should have higher salary accommodation, transport facility nurseries, day care facility, allowance for attending CME’s and access to journals and books and 15-20% mark for PG admission. The PHC should have adequate investigation facilities, medicines and required staff. To ensure the availability of MBBS doctors, and Indian National Medical Services can be formed to enlist a panel of MBBS doctors who will work in rural areas at least for one or two years on a package basis.
Indian National Medical Services
Will have a panel of MBBS doctors who can be posted in very difficult and difficult PHCs. They should have a package with higher pay, Doctors’ quarters, transportation facility, allowance for attending CMEs, availability of e-journals and books to prepare for PG , Nursery and Day Care Centre for children and 15-20% additional marks for PG Entrance. They can serve the rural PHC for one or two years. They will be posted in any PHC where there is a vacancy.
As a long term solution District Hospitals are to be upgraded into Medical Colleges to address the need for more MBBS doctors.
New Medical Colleges should be started in Public Sector particularly in regions where Medical College are not present to correct the geographical mal-distribution of Medical college
Licentiate examination
The national medical commission bill in Chapter IV clause 15 (1), (2), (3), (4), (5) mention about Uniform national licentiate examination for granting licence to practice modern medicine.
Dr Vinay Aggarwal, Ex President,  IMA, said, “ Qualifying licentiate examination no MBBS person will be enrolled in the National register and will not be entitled to practice or do further post graduate courses. Further the standard and backward communities would find it great difficulty to clear the exam. This would cause a great harm to them because they would neither be able to practice not would be able to take admission to PG courses”
IMA, said, “ Qualifying licentiate examination no MBBS person will be enrolled in the National register and will not be entitled to practice or do further post graduate courses. Further the standard and backward communities would find it great difficulty to clear the exam. This would cause a great harm to them because they would neither be able to practice not would be able to take admission to PG courses”
“ In addition even the students learning in medical colleges situated in remote areas as well as backward areas will also suffer in a similar manner. The net result would be that thousands of students passing their MBBS examination belonging to socio economically backward communities and from backward areas including north-east region would not be able to practice or seek admission to PG courses for want of clearance of the licentiate examination because of its higher standards,” he added.
It is worthwhile to note the neither the Parliamentary standing committee nor the Ranjit Roy Chaudhaury Committee had recommended such a licentiate exam n their respective reports.
The Hon’ble Parliamentary Standing Committee in its report in Page 94 submits:
“The committee takes note of the submission that today’s graduate doctor after doing his internship is to confident of practicing because his entire period of one year internship goes into studying for PG entrance examination. The committee observes that skill training which is very important for a medical professional is not being acquired during internship. The committee therefore recommends that the PG entrance exam should be held immediately after final MBBS examination so that the graduate doctor could concentrate on practical skills during internship.”
The Ranjit Roy Chaudhury Committee, in its report regarding UG Board, in point no. 15 of UG Board HAS SPECIFICALLY MENTIONED THAT THE FINAL ECAM WILL BE CONDUCTED BY RESPECTIVE UNIVERSITIES and the board will work in close collaboration with the universities to ensure that the assessment norms are being followed. (Page no. 118 of Hon’ble Parliamentary Standing Committee report; Appendix Ranjit Roy Chaudhurty Committee Report)
 Dr R N Tandon, Secretary General, IMA, said, “Hence the PG NEET and Exam for Government recruitment may be conducted immediately after the final MBBS examination, before commencement of internship, but it should not be linked to licence to practice..”
Dr R N Tandon, Secretary General, IMA, said, “Hence the PG NEET and Exam for Government recruitment may be conducted immediately after the final MBBS examination, before commencement of internship, but it should not be linked to licence to practice..”
Indian Medical Association (IMA) requests the Hon’ble Parliamentary Standing Committee to make necessary changes in Chapter IV, Clause clause 15 (1), (2), (3), (4), (5), so that the concept of National Licentiate Exam is dropped.
To address the concern about the lack of uniform standard of MBBS graduates, The final year MBBS examination can be conducted as a common examination.
All common examinations including NEET and PG NEET should be under an examination board outside NMC except final year MBBS common examination.
Lack of representative character:
The Bill seeks to introduce a bureaucratic setup in the National Medical Commission with most of the members nominated by the central government, There are only 5 elected members from the registered Modern Medical practitioners from the state register
 Dr K K Aggarwal, Ex President, IMA, said, “Instead of Five elected members one each should be elected from each state/ Union Territory from amongst the registered medical practitioners of Modern Medicine. IMA proposes one elected member from registered practitioners of Modern Medicine from each State. 50% of the elected members should be members of the autonomous Boards instead of having all nominated members. Board should consist of at least 6-8 members in total instead of only 3 members as suggested in the NMC Bill.”
Dr K K Aggarwal, Ex President, IMA, said, “Instead of Five elected members one each should be elected from each state/ Union Territory from amongst the registered medical practitioners of Modern Medicine. IMA proposes one elected member from registered practitioners of Modern Medicine from each State. 50% of the elected members should be members of the autonomous Boards instead of having all nominated members. Board should consist of at least 6-8 members in total instead of only 3 members as suggested in the NMC Bill.”
Representation for IMA in NMC:
IMA has been a member of both MCI and NBE, hence National President of IMA (or his nominee) should be included among the Ex Officio Members, by virtue of being the president of 206 lakhs modern medicine doctors.
Clause 11. (1) The Central Government shall constitute an advisory body to be known as the Medical Advisory Council.
(2) The Council shall consist of a Chairperson and the following Members, namely:-
a)The Chairperson of the Commission shall be the ex officio Chairperson of the Council;
b)Every Member of the Commission shall be the ex officio Members of the Council;
c)One Member to represent each State, who is the Vice-chancellor of a health University in the State, to be nominated by that State Government;
d)One Member to represent each Union territory, who is the Vice-Chancellor of a health University in that Union territory, to be nominated by the Ministry of Home Affairs in the Government of India;
e)The Chairman, University Grants Commission;
f)The Director, National Assessment and Accreditation Council;
g)For Members to be nominated by the Central Government from amongst persons holding the post of Director in the Indian Institutes of Technology, Indian Institutes of Management and the Indian Institute of Science:
Provided that if there is no health University in any State or Union Territory, the Vice-Chancellor of a University within that State or Union territory having the largest number of medical colleges affiliated to it shall be nominated by the State Government or by the Ministry of Home Affairs in the Government of India. Provided further that if there is no University in any Union territory, the Ministry of Home Affairs shall nominate a Member who possesses such medical qualification and experience as may be prescribed.
 Dr. Ravi Wankhedkar, said, “IMA demands that the National Medical Commission should not have non medical persons as members. The services of non medical experts and be utilized as part time consultants. “
Dr. Ravi Wankhedkar, said, “IMA demands that the National Medical Commission should not have non medical persons as members. The services of non medical experts and be utilized as part time consultants. “
Directions to State Medical Councils:
The proposed Bill at section 10(1)(f) authorizes the commission to take such measures as may be necessary to ensure compliance by the State Medical Councils of the guidelines framed and regulations made under this Act for their effective functioning under this Act
The proposed Bill under section 30(2) entitles that Central Govt. to give direction to the State Medical Council for dispensation of task under their jurisdiction. All these provisions shall take away the autonomy vested with the State Medical Council and make them subservient to the Central Govt and NMC. This would be a great prejudice caused to the State Medical Councils and violation of principles of FEDERAL STSTEM.
 Dr Manglesh Pate, Joint Secretary, said,” IMA demands the autonomy of the State Medical Council should be retained.” Composition of Medical Advisory Council Under section 11(1) of the proposed Bill the Central Govt. is required to constitute an Advisory Body to be known as the Medical Advisory Council.
Dr Manglesh Pate, Joint Secretary, said,” IMA demands the autonomy of the State Medical Council should be retained.” Composition of Medical Advisory Council Under section 11(1) of the proposed Bill the Central Govt. is required to constitute an Advisory Body to be known as the Medical Advisory Council.
The composition of the said Council stipulated at section 11(2) at its sub section (c ) provides for that one member to represent each State who is the Vice Chancellor of a health University in that State to be nominated by that State Govt. However, at a proviso it brings out that “if there is no health university in any state or Union Territory the Vice Chancellor of a university within that state or Union Territory having the largest number of medical college affiliated to it shall be nominated by the State Govt. or the ministry of home affairs in the Govt. of India.
A health sciences university apart form including medical colleges has under its ambit colleges of other stream of health sciences as well. The vice Chancellor of a health sciences university of a State therefore necessarily would not be a person possessing qualification in modern medicine.
Further, in case of non-health sciences universities, where under apart from medicine faculty there are several other faculties, the Vice Chancellor of such a university to which maximum number of medical colleges would be affiliated in the State could be a person who may not be even from the stream for health science. As such, the said proviso opens doors for representation of people as Vice Chancellor not only from non-medical faculty amongst health sciences but form the non-health sciences faculty as well.
“IMA demands that instead of VC of the university, a Modern Medical Doctor who should be elected form among the syndicate members of the university should represent the university,” Dr Manglesh, said.
Accreditation Council and National Medical Grants Commission IMA also demands the formation of Accreditation Council and Medical Grants Commission outside NMC ACCREDITATION COUNCIL- as is in existence even for art and science colleges should be added to NMC. The inspection at the time of starting a medical college will be assessing only infrastructural facilities and manpower. But the accreditation council assess the standards of medical teachings, pass percentage and student performance which in effect will assure uniform minimum standards in medical education and there will be no need for NEXT (National Exit Exam). NATIONAL MEDICAL GRANTS COMMISSION also should be added in NMC to encourage research, teachers’ career advancement, and funding teachers training programs Penalty for non-compliance should be fixed:
The penalty for non compliance varies from 5 crores to 100 crores which again opens the gates for corruption. The penalty should be fixed.
Fee Fixation:
In 60% medical seats, fees fixation is left the management which will make medical education unaffordable to socio economically weaker sections of the society. The Management seats should be limited to 15%. The proposed Medical Grants Commission can support private medical colleges even financially.
MCI Act can be amended
These proposed amendments can be incorporated in the present MCI Act or through NMC. Indian medical Association request the Parliamentary Standing Committee to consider the above mentioned facts and modify the bill to achieve its aim of providing a medical education system that ensues availability of adequate and high quality medical professionals with zeal in research, orientation in health needs of the country with high ethical standards.
 Dr. Vijay Agarwal, President, Consortium of Accredited Healthcare Organization (CAHO) and Advisor to Max Healthcare, Replacing MCI with another body could have made sense only after it was analyzed as to why was MCI not working and what makes one believe that the new body will not be “corrupt”. It is very interesting that MCI was suspended and replaced by handpicked professionals with integrity for three long years from 2010 to 2013.
Dr. Vijay Agarwal, President, Consortium of Accredited Healthcare Organization (CAHO) and Advisor to Max Healthcare, Replacing MCI with another body could have made sense only after it was analyzed as to why was MCI not working and what makes one believe that the new body will not be “corrupt”. It is very interesting that MCI was suspended and replaced by handpicked professionals with integrity for three long years from 2010 to 2013.
Was any improvement perceived? None to the eyes of many and that was the reason it was not continued with. Replacing one body with another will NOT serve any purpose unless we do a brainstorming about the underlying reasons as to why even the Government appointed Board could not redeem the image of MCI.
A number of medical colleges are being owned by political masters and they have been having indirect control over MCI and now in the new proposed body they can have more effective control!! Unless this conflict of interest is identified and neutralized no “institution” is likely to be effective…

