Retain Your Sight
 If you are a diabetic, finding and treating the eye disease early, before it causes vision loss or blindness, is in your best interests.
If you are a diabetic, finding and treating the eye disease early, before it causes vision loss or blindness, is in your best interests.
By Dr Shishir Narayan
If you experience spots or dark strings, blurred, fluctuating, impaired colour and dark or empty areas in your vision, then you may suffer from diabetic retinopathy. In common parlance, diabetic retinopathy is a diabetes complication that affects eyes. If not treated on time, it can cause blindness.
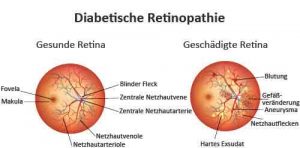
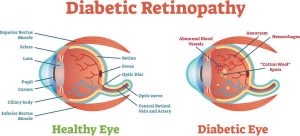
Diabetic retinopathy is the most common cause of vision loss among people with diabetes and a leading cause of blindness among working-age adults. Basically, diabetic retinopathy is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina).
 Effective treatments are available to prevent vision loss from diabetic retinopathy. The most opportune time for these treatments is before any vision has been lost, since even advanced diabetic retinopathy can be present when a person has no vision complaints or problems.
Effective treatments are available to prevent vision loss from diabetic retinopathy. The most opportune time for these treatments is before any vision has been lost, since even advanced diabetic retinopathy can be present when a person has no vision complaints or problems.
Elevated levels of blood glucose can damage the body in various ways, including harming the blood vessels in your eyes. Diabetes can affect the lining of the blood vessels in your eyes, causing them to thicken and develop leaks. Poor circulation in the retinal vessels can compound these problems by causing the production of fragile new vessels.
 Symptoms of retinopathy
Symptoms of retinopathy
At first, diabetic retinopathy may cause no symptoms or only mild vision problems. Eventually, it can cause blindness. The condition can develop in anyone who has type-I or type-II diabetes. The longer you have diabetes and the less controlled blood sugar is, the more likely you are to develop this eye complication.
You might not have symptoms in the early stages of diabetic retinopathy. As the condition progresses, diabetic retinopathy symptoms may include dark strings, blurred, fluctuating, impaired colour and dark or empty areas in vision. Diabetic retinopathy usually affects both eyes.
With proper treatment plan, you can prevent vision loss. If you have diabetes, see your eye doctor for a yearly eye exam with dilation even if your vision seems fine. Pregnancy may worsen diabetic retinopathy, so if you are pregnant, your eye doctor may recommend additional eye exams throughout your pregnancy. Contact your eye doctor right away if your vision changes suddenly or becomes blurry, spotty or hazy.
Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply. As a result, the eye attempts to grow new blood vessels. But these new blood vessels don’t develop properly and can leak easily.
There are two types of diabetic retinopathy:
 Early diabetic retinopathy
Early diabetic retinopathy
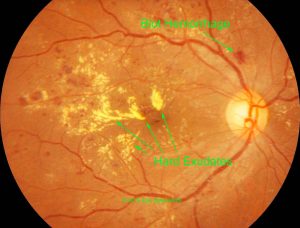
In this more common form — called No Proliferative Diabetic Retinopathy (NPDR) — new blood vessels are not growing. The walls of the blood vessels in retina weaken. Tiny bulges protrude from the vessel walls of the smaller vessels, sometimes leaking fluid and blood into the retina. Larger retinal vessels can begin to dilate and become irregular in diameter, as well. NPDR can progress from mild to severe, as more blood vessels become blocked.
After 20 years of diabetes, most persons with diabetes will shows some signs of NPDR, which is generally not sight-threatening itself unless macular edema is present.
 Proliferative diabetic retinopathy
Proliferative diabetic retinopathy
It is a more serious stage of retinopathy and poses a greater risk of hemorrhage into the vitreous humor, the clear gel that fills the centre of the eye, or detachment of the retina leading to severe vision loss. Diabetic macular edema can occur with either non proliferative or proliferative diabetic retinopathy.
Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macula) begins to swell (macular edema), a condition that requires treatment.
Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy. In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina, and can leak into the clear, jelly-like substance that fills the centre of your eye (vitreous).
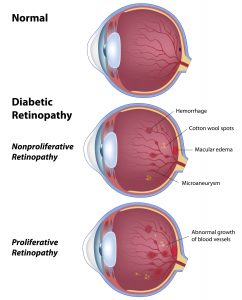 Ultimately, scar tissue stimulated by the growth of new blood vessels may cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure may build up in the eyeball. This can damage the nerve that carries images from eye to brain resulting in glaucoma. The longer you have diabetes, the greater risk of developing diabetic retinopathy. Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications can lead to serious vision problems.
Ultimately, scar tissue stimulated by the growth of new blood vessels may cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure may build up in the eyeball. This can damage the nerve that carries images from eye to brain resulting in glaucoma. The longer you have diabetes, the greater risk of developing diabetic retinopathy. Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications can lead to serious vision problems.
In vitreous hemorrhage, the new blood vessels may bleed into the clear, jelly-like substance that fills the centre of your eye. If the amount of bleeding is small, you might see only a few dark spots. In more-severe cases, blood can fill the vitreous cavity and completely block your vision. Vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
In retinal detachment, the abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss.
New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up (glaucoma). This pressure can damage the nerve that carries images from your eye to your brain (optic nerve). Finally. The 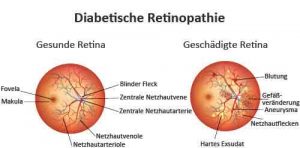 patients of diabetic retinopathy, glaucoma or both can lead to complete vision loss.
patients of diabetic retinopathy, glaucoma or both can lead to complete vision loss.
Treatment of retinopathy
Laser photocoagulation is used to seal leaking blood vessels that may cause edema or swelling in the macula area of the eye. Laser surgery and appropriate follow-up care can reduce the risk of blindness by 90 percent. The primary goal of laser surgery is to prevent further vision loss and not to restore vision that has already been lost, which is why finding diabetic retinopathy early is the best way to prevent vision loss.
Laser treatment generally is not painful but may cause some temporary discomfort. The laser surgery is done on an outpatient basis in the ophthalmologist’s office. After treatment, some people may experience a slight decrease in vision or it may become more difficult to adjust to darkness, a side effect that diabetes itself may cause. But the overall benefits of the laser treatment far outweigh these relatively minor drawbacks. Serious cases of eye damage in people with diabetes can be treated. If a hemorrhage does occur and vision is lost, or if the scar tissue threatens to detach the retina from the back of the eye, vitrectomy surgery can successfully restore vision.
Finding and treating the eye disease early, before it causes vision loss or blindness, is the best way to control eye disease in people with diabetes. So if you have diabetes, make sure you receive a comprehensive dilated eye examination at least once a year. Also, keep good control of your glucose levels and other health problems such as high blood pressure, kidney disease, and elevated cholesterol.
(The author is Senior Eye Consultant, Eye Trust, Ghaziabad and associated with Shroff Eye Hospital, New Delhi)

