Towards TB Free India
TB Free India is only possible if we ensure that our panchayat and blocks are declared TB free. For that, the Government has adequately provisioned drugs and diagnostic in every part of the country…
By Abhigyan/Abhinav
TB and under nutrition can cause a vicious cycle of worsening disease and under nutrition. Under nutrition is linked to a number of serious outcomes related to TB disease….
 What is TB?
What is TB?
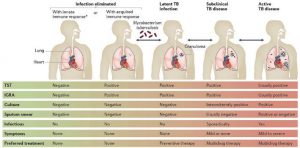
TB is an abbreviation of the word tuberculosis and is how people often refer to the disease. TB is caused by bacteria called Mycobacterium tuberculosis (M.tuberculosis). Most individuals with active TB experience weight loss. Weight loss among people with TB can be caused by several factors, including reduced food intake due to loss of appetite, nausea and abdominal pain.
Just a few years ago it was believed that TB was an old disease, and that it was no longer a problem in humans. But now because of such issues as drug resistance and HIV, it has become a major worldwide problem again. Globally, more people die from the disease than from any other infectious disease.
How do you get TB?
TB is spread from one person to another through the air. You get TB by breathing in TB bacteria that are in the air. Bacteria get released into the air by someone who already has the bacteria in their body.
For a long time it has been known that there is a link between TB and malnutrition. There is a two-way link between TB & malnutrition.TB makes malnutrition worse, and malnutrition makes TB worse.
TB and malnutrition
Malnutrition is often considered to refer to people having an insufficient intake of food. But it strictly refers to people having either under nutrition or equally people who have too much food, that is, people who are obese. So, in the context of TB it is usual to refer to under nutrition, which is people getting insufficient nutrients from their food.
Equally under nutrition weakens the body’s ability to fight disease. So under nutrition increases the likelihood that latent TB will develop into active TB disease. Although there is a clear link between active TB and under nutrition, in no way does malnutrition or under nutrition cause TB on its own. TB is only ever caused by TB bacteria. Food insecurity and malnutrition in people who are in close contact of a patient with active TB increases their risk of developing TB. Persons with TB should aim to have three meals and three snacks each day to increase the amount of food they eat. There is increasing evidence that under nutrition in patients with active TB is associated with an increased frequency and severity of disease and indeed a two to four fold increase in mortality. There is also a five fold risk of drug induced liver damage.
A less than ideal weight gain during TB treatment also increases the risk of long term relapse even after initial cure. Under nutrition has also been associated with malabsorption of key anti TB drugs.
 Consultative Meeting on TB
Consultative Meeting on TB
Consultative Meeting discussed three dimensions of the response to TB – key and priority populations, law and human rights and gender – and released assessment reports on the same in New Delhi recently. The meeting was organised by REACH and supported by the Stop TB Partnership. Speaking at the meeting, Deputy Director General (TB), Dr. K. Sachdeva said, “The person-centred approach to TB is already in the new National Strategic Plan (NSP) for TB elimination. We take cognizance of these dimensions that need to be addressed and welcome these findings.”
The three tools – Data for Action
Framework for Key Populations, Gender and Legal Environment Assessment developed by the Stop TB Partnership provided the guiding framework for undertaking rapid assessments of the three different dimensions. An increased focus on these aspects has the potential to not just increase case detection and treatment outcomes but also improve the overall quality of care.
TB affects an estimated three million women every year and remains among the top five leading causes of death among adult women globally. Although more men are affected by TB, women experience the disease differently, and gender disparities could play a significant role in how men and women access healthcare in the public and private sectors.
The Gender Assessment Tool is a guiding framework to undertake a gender analysis of the existing TB epidemic and response. Through this framework, existing data and information about TB in India will be collated and analyzed through a gender lens Dr Sundari Mase, WHO and Expert Advisory Group Member, CRG Assessments, said, “Globally, one-third of the people diagnosed with TB are women. Gender and TB is an area where India can take the lead. When women are dying of TB, there is a cascading impact on children, families and society.”
The National Strategic Plan (NSP) for TB elimination 2017-2025, for the first time, included a separate chapter on Priority Populations, who are primarily vulnerable, underserved or populations at risk of TB infection and illness due to various factors. In this context, the data framework tool provides an opportunity to understand better how TB impacts key and priority populations in terms of both burden and access to services. “For the vulnerable populations, steps should be tailor made. One size does not fit all. Certain things need to be fixed as per the needs of a community – whether they are miners, slum dwellers or people living with HIV,” Mona Balani of Touched By TB said.
The right to health from a human rights perspective is indivisible and interdependent on other rights such as the right to food, housing, right to a healthy environment, right to work and rights at work, right to education etc. The Legal Environment Assessment tool reviews existing legislations and policies that affect rights from a health perspective,and the existing legislations and policies that could possibly create barriers for access to TB services.
Health Ministry’s new initiatives to combat TB
According to Preeti Sudan, Secretary (Health) Govt of India,we are already aligned with world TB treatment protocols. India has a mission to end TB by 2025, through community participation, involving civil societies and other stakeholders. She further stated that the global target to end TB is 2030 but we will end it by 2025. “This is a tall order but I am confident that if we all work together, if all the partners combine together and we ensure full treatment is given on regular basis we can show the world this can be achieved. I am confident of this and my confidence is backed by our success in eradicating Polio.”
At a recently held function, the Health Secretary also released the TB INDIA 2018 Report and National Drug Resistance Survey Report. She also launched the Nikshay Aushadi Portal and shorter regimen for Drug Resistant TB. Preeti Sudan commended the TB warrior, Shri Suman, a graduate student who narrated his experience living with TB. The Health Secretary stated that early identification and complete treatment of TB is a key to achieving our goal of TB elimination. We need many TB warriors like Suman to fight against this disease and spread positive message across the communities to burst the myths and misconceptions around TB.
Addressing the participants, the Health Secretary further stated that the Prime Minister has called for ‘TB Mukth Bharat’ which can only possible if we ensure our panchayat and blocks are declared TB free. “For that Government has adequately provisioned drugs and diagnostic in every part of the country,” she added.
 Also present at the event were Dr B D Athani, DGHS, Sanjeeva Kumar, Additional Secretary (Health), A. K. Jha, Economic Advisor, Ministry of Health & Family Welfare, Vikas Sheel, Joint Secreatry, Dr. Sunil Khaparde, DDG(TB), and other senior officers of the Health Ministry, representatives of WHO and other development partners.
Also present at the event were Dr B D Athani, DGHS, Sanjeeva Kumar, Additional Secretary (Health), A. K. Jha, Economic Advisor, Ministry of Health & Family Welfare, Vikas Sheel, Joint Secreatry, Dr. Sunil Khaparde, DDG(TB), and other senior officers of the Health Ministry, representatives of WHO and other development partners.
In addition to the well-known risk factors contributing to the rise of tuberculosis cases in India, like human immune deficiency virus/acquired immune deficiency syndrome (HIV/AIDS), poor nutritional status, and young age, realization that other emerging factors like diabetes mellitus, indoor air pollution, alcohol abuse, tobacco smoke are also fuelling the epidemic, adding more complexities to tuberculosis control and making the task onerous. Individually and in combination, risk factors tend to increase the burden two to three times.
Unless addressed concurrently, these numbers are likely to overwhelm the tuberculosis control programme and annul its efforts. The eight states of the North Eastern region characterized by hilly, forested area, sparsely inhabited mainly by tribal populations also share high prevalence of emerging risk factors for tuberculosis.
India has set itself a target of elimination of tuberculosis by 2025. To achieve the target in the North Eastern states, special resources would be needed to be put in place for controlling these risk factors as well. A comprehensive integrated approach taking help of other departments in health sector and beyond is critical.
There are two risk factors like diabetes mellitus and tobacco smoking which impact a larger section of North-Eastern population and accelerate progression of tuberculosis disease. Some of the states here have highest prevalence of HIV in India, notably Manipur (1.15%), Nagaland and Mizoram (0.7–0.8%).
India has an average of 0.26%. People with HIV have a 20–30 times higher risk of developing active tuberculosis, which is more of the extra pulmonary type and throws up challenges of diagnosis and management.
Tobacco consumption is highest in this region of the country. On an average people in NE smoke more tobacco than the rest of India.
Mizoram and Meghalaya have a prevalence of over 60%, Tripura follows at 40%. India’s average is around 26%. One in four Mizo women smokes, whereas average for India is 1 per hundred. Smokers are two-three times at higher risk of developing tuberculosisthan non-smokers. The disease is more severe. A regular smoker has twice the risk of getting the disease again, recurrences are more often. If an HIV infected individual also smokes, the risk increases three folds.
Diabetes is the third risk factor. Results of an India-wide show high prevalence of pre-diabetes especially amongst the urban poor in the states of Arunachal Pradesh, Manipur, and Meghalaya which is of major concern. Diabetes again increases the risk of tuberculosis to three folds and the risk of multi drug resistant (MDR) among diabetics who get TB is 2–8 times higher. The progression of the disease is rapid. And it develops more frequently when the diabetes control is poor.
What does all this mean to the tuberculosis elimination programme? Elimination of TB means stopping transmission. That is reach every person suspected to have tuberculosis, get diagnosis confirmed, and if positive put on appropriate treatment and help to complete the therapy. Given the difficult terrain and hard to reach population, more resources would be needed. Health workers may have to travel long distances to bring one patient under treatment successfully. Finding TB cases is critical.
 Modelling studies have shown that if the case detection is increased by 25%, it can translate in to about 40% reduction in mortality, the prevalence decreases by about 30% and the reduction of incidence cases is by more than 20% in 10 years. For persons with chest symptoms, sputum examination for acid-fast bacilli (AFB) is the recommended test. Acid fast staining of sputum for AFB performs poorly as a screening test. Its sensitivity is poor. The cartridges based nucleic acid amplification test (Cartridge Based Nucleic Acid Amplification test, CB-NAAT) is now available at the district level as it needs a controlled temperature and dust free environment.
Modelling studies have shown that if the case detection is increased by 25%, it can translate in to about 40% reduction in mortality, the prevalence decreases by about 30% and the reduction of incidence cases is by more than 20% in 10 years. For persons with chest symptoms, sputum examination for acid-fast bacilli (AFB) is the recommended test. Acid fast staining of sputum for AFB performs poorly as a screening test. Its sensitivity is poor. The cartridges based nucleic acid amplification test (Cartridge Based Nucleic Acid Amplification test, CB-NAAT) is now available at the district level as it needs a controlled temperature and dust free environment.
A nucleic acid amplification test (True Nat MTB), a chip based test has been developed by an Indian company. It is reported to have good sensitivity and specificity. It has recently been validated in 100 designated microscopy centres in 50 districts in 10 states in which 18,000 samples have been tested. This battery operated test takes around an hour to give the result whether a sputum sample is positive for TB, for positive samples resistance can be determined in another hour’s time. It does not require dust proof air-conditioned environment. It is projected as a test to be used at primary health centre (PHC) level. If it is found to have an acceptable sensitivity and specificity, this test should be deployed in the NE states on a priority basis.
Relying on symptoms-screen alone may be contributing to delayed diagnosis of tuberculosis. Using chest X-rays (CXR) as a pre-screen test can reduce numbers needed to test for each case of tuberculosis. Abnormal CXRs could, therefore, be key to active case finding by identifying cases that otherwise would have not have been diagnosed by conventional, passive case finding, Today, CXR is becoming more accessible in remote settings due to technological advances such as digital imaging instead of film-processed images. The sensitivity of CXR has been shown to increase if computer – aided diagnosis (CAD) software is used to analyse digital images. It gives a probability percentage consistent with TB. It could possibly be used as a ‘filter’ in TB screening to identify that gets tested by CB NAAT (GeneXpert).
We need a locally available and economic version of the CAD4TB which would help in improving diagnosis especially in areas where a radiologist is not available to interpret the CXR. Diabetes triples the risk for active tuberculosis, thus the increasing burden of type 2 diabetes will further burden the TB elimination programme. An epidemiological model in Indiaindicates that diabetes mellitus may account for 15% of TB cases. The International Diabetes Federation has predicted an increase in diabetes prevalence to 10% world wide by 2035. Modelling exercises have predicted that if such an increase does happen it could undercut the decrease in new cases of tuberculosis by about 3%. Some believe that increase in the prevalence of diabetes in India has contributed in part to a negligible reduction in new cases oftuberculosis between 1988 and 2008.
Diabetic tuberculosis patients have a higher risk of treatment failure, death, and recurrent tuberculosis as compared to non-diabetic tuberculosis patient. Poorly controlled diabetes increase the risk of tuberculosis and leads to unfavourable tuberculosis treatment outcomes. Researchers have long known that diabetes patients have higher blood sugar levels making their disease difficult to control and putting them at greater risk of developing complications. A bidirectional screening for tuberculosis and diabetes mellitus at hospital and community level has been shown to be feasible and effective. Such a screening should be piloted at hospital and community level and scaled- up. This presents a unique opportunity to capture persons presenting with either of these two conditions as potential targets for screening and treatment. Patients with diabetes often present with atypical symptoms and pose hurdles in diagnosing tuberculosis. Clinical management of patients with both diseases can be difficult. Tuberculosis patients with diabetes have a lower concentration of tuberculosis drugs and a higher of drug toxicity than tuberculosis patients without diabetes. Besides drug treatments for tuberculosis and diabetes, other interventions, such as education, intensive monitoring, and lifestyle interventions, might be needed, especially for patients with newly diagnosed diabetes or those who need insulin.
Modelling study analysed the potential effect of diabetes on tuberculosis epidemiology in 13 countries with high TB burden. The study estimated the tuberculosis burden that can be reduced by alternative scenarios of diabetes lowering the prevalence of diabetes by an absolute level of 6.6–13.8% could accelerate the decline of tuberculosis incidence by an absolute level of 11.5–25.2% and tuberculosis mortality by 8.7–19.4%. If interventions reduce diabetes incidenceby 35% by 2025, 7.8 million tuberculosis cases and 1.5 million tuberculosis deaths could be averted by 2035.
The evidence for an regular tobacco smoking increases risk of TB in active smokers is well established. There is alsosome evidence that second hand smoking (passive smoking) is a risk factor for developing tuberculosis especially in children 0–5 years. When exposed to second hand smoke, household/ environmental factors (crowding, biomass fuel burning) may increase risk for developing tuberculosis.
In addition, smoking has been associated with cavitary lesions, bacillary load, smear conversion delay, and high risk of reactivation and death during or after treatment. Smoking rates are high among men in North Eastern states, and, together with rising rates of diabetes, the risk of progression to tuberculosis disease will also increase. Interventions like smoking cessation and early screening for tuberculosis can be advocated, but the impact of interventions in reducing TB risk remains negligible at population level. Both active and passive smoking increase susceptibility to TB infection, progression to active TB disease and the risk of adverse anti-TB treatment outcomes. Systematic reviews suggest that the risk of TB disease among smokers is increased two to threefold compare with people who have never smoked. Tobacco control and smoking cessation among people with diabetes and tuberculosiscan therefore play an important role in limiting the burden of TB. It is also known that diabetic smokers have more than 5-fold increased risk of pretreatment positive smears than do non- diabetic non-smokers.
This is a remarkable joint effect of diabetes and smoking that increased risk of tuberculosis transmission. Against the background of risk factors fuelling the epidemic of tuberculosis in India, a critical assessment of the tuberculosis control programme (like strengths, weaknesses, opportunities and threats (SWOT) analysis) especially in the North-Eastern region would be helpful in identifying the areas that need strengthening to deal with these risk factors, and the resultant possible increase in number of active tuberculosis patients. From a health systems point of view, issues such as delays in diagnosis, initiation of appropriate treatment and its successful completion would be crucial. Experience from the combating combined HIV/TB disease would be helpful. But more operational research would be needed to tackle diabetes and tobacco smoking.
The Revised National Tuberculosis Control Program (RNTCP) would need to solicit assistance from other programmes within and outside the health sector to develop integrated comprehensive approach in meeting the targets of tuberculosis elimination in the North Eastern region.

