Removing The Stigma
Significantly, to end discrimination against HIV patients, the Ministry of Health and Family Welfare has recently issued a notification for bringing the Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (Prevention and Control) Act, 2017 in force from 10th September, 2018
By Amresh K Tiwary
 India has the third largest HIV epidemic in the world. However, although overall prevalence remains low, even relatively minor increases in HIV infection rates in a country of more than one billion people translate into large numbers of people becoming infected.
India has the third largest HIV epidemic in the world. However, although overall prevalence remains low, even relatively minor increases in HIV infection rates in a country of more than one billion people translate into large numbers of people becoming infected.
With an aim to prohibit discrimination against individuals who are diagnosed with HIV/AIDS, the Ministry of Health and Family Welfare has recently issued a notification for bringing the Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (Prevention and Control) Act, 2017 in force from 10th September, 2018.
The Act, safeguards the rights of people living with HIV and affected by HIV. The provisions of the Act address HIV-related discrimination, strengthen the existing programme by bringing in legal accountability, and establish formal mechanisms for inquiring into complaints and redressing grievances.
The Act seeks to prevent and control the spread of HIV and AIDS, prohibits discrimination against persons with HIV and AIDS. The Act lists various grounds on which discrimination against HIV positive persons and those living with them is prohibited.
These include the denial, termination, discontinuation or unfair treatment with regard to:
- Employment,
- Educational establishments,
- Health care services,
- Residing or renting property,
- Standing for public or private office,
- Provision of insurance (unless based on actuarial studies). The requirement for HIV testing as a pre-requisite for obtaining employment or accessing health care or education is also prohibited.
Every HIV infected or affected person below the age of 18 years has the right to reside in a shared household and enjoy the facilities of the household. The Act also prohibits any individual from publishing information or advocating feelings of hatred against HIV positive persons and those living with them.
The number of people who inject drugs (sometimes referred to as PWID) living with HIV in India is rising. The prevalence rate remained steady at around 7% between 2007 and 2013, but was estimated at 9.9% in 2015.
 As per provisions of the Act, a person between the age of 12 to 18 years who has sufficient maturity in understanding and managing the affairs of his HIV or AIDS affected family shall be competent to act as a guardian of another sibling below 18 years of age to be applicable in the matters relating to admission to educational establishments, operating bank accounts, managing property, care and treatment, amongst others. As per the provisions of the Act, every person in the care and custody of the state shall have right to HIV prevention, testing, treatment and counseling services.
As per provisions of the Act, a person between the age of 12 to 18 years who has sufficient maturity in understanding and managing the affairs of his HIV or AIDS affected family shall be competent to act as a guardian of another sibling below 18 years of age to be applicable in the matters relating to admission to educational establishments, operating bank accounts, managing property, care and treatment, amongst others. As per the provisions of the Act, every person in the care and custody of the state shall have right to HIV prevention, testing, treatment and counseling services.
What is AIDS
AIDS (Acquired Immuno Deficiency Syndrome) is a syndrome caused by a virus called HIV (Human Immuno Deficiency virus). The disease alters the immune system, making people much more vulnerable to infections and diseases. This susceptibility worsens if the syndrome progresses.HIV is found throughout all the tissues of the body but is transmitted through the body fluids of an infected person (semen, vaginal fluids, blood, and breast milk).
 What is HIV?
What is HIV?
HIV is a virus that attacks immune cells called CD-4 cells, which are a subset of T cells. AIDS is the syndrome, which may or may not appear in the advanced stage of HIV infection. HIV infection can cause AIDS to develop. However, it is possible to contract HIV without developing AIDS. Without treatment, HIV can progress and, eventually, it will develop into AIDS in the vast majority of cases HIV is a retrovirus that infects the vital organs and cells of the human immune system.The virus progresses in the absence of antiretroviral therapy (ART) – a drug therapy that slows or prevents the virus from developing.
The rate of virus progression varies widely between individuals and depends on many factors.These factors include the age of the individual, the body’s ability to defend against HIV, access to healthcare, the presence of other infections, the individual’s genetic inheritance, resistance to certain strains of HIV, and more.
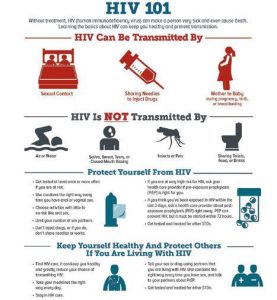
How is HIV transmitted?
Sexual transmission — it can happen when there is contact with infected sexual fluids (rectal, genital, or oral mucous membranes).
This can happen while having sex without a condom, including vaginal, oral, and anal sex, or sharing sex toys with someone who is HIV-positive.
Perinatal transmission — a mother can transmit HIV to her child during childbirth, pregnancy, and also through breastfeeding.
Blood transmission — the risk of transmitting HIV through blood transfusion is extremely low in developed countries, thanks to meticulous screening and precautions. However, among people who inject drugs, sharing and reusing syringes contaminated with HIV-infected blood is extremely hazardous.
Symptoms
For the most part, the later symptoms of HIV infection are the result of infections caused by bacteria, viruses, fungi, and/or parasites. These conditions do not normally develop in individuals with healthy immune systems, which protect the body against infection.
Early symptoms of HIV infection
Some people with HIV infection have no symptoms until several months or even years after contracting the virus. However, around 80 percent may develop symptoms similar to flu 2–6 weeks after catching the virus. This is called acute retroviral syndrome.
The symptoms of early HIV infection may include fever, chills, joint pain, muscle aches, sore throat, sweats (particularly at night), enlarged glands, a red rash, tiredness, weakness, unintentional weight loss and thrush.
It is important to remember that these symptoms appear when the body is fighting off many types of viruses, not just HIV. However, if you have several of these symptoms and believe you could have been at risk of contracting HIV in the last few weeks, you should take a test.
 Asymptomatic HIV
Asymptomatic HIV
In many cases, after the initial symptoms disappear, there will not be any further symptoms for many years.
During this time, the virus carries on developing and damaging the immune system and organs. Without medication that stops HIV replicating, this process of slow immune depletion can continue, typically for an average of 10 years. The person living with HIV often experiences no symptoms, feels well, and appears healthy.
For people who are taking antiretroviral and are rigidly compliant, this phase can be interrupted, with complete viral suppression. Effective antiretroviral arrest on-going damage to the immune system.
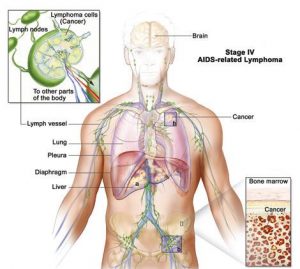
Late-stage HIV infection
If left untreated, HIV weakens the ability to fight infection. The person becomes vulnerable to serious illnesses. This stage is known as AIDS or stage 3 HIV.
Symptoms of late-stage HIV infection may include blurred vision, diarrhea which is usually persistent or chronic, dry cough, fever of above 100 °F (37 °C) lasting for weeks, night sweats, permanent tiredness, shortness of breath (dyspnea), swollen glands lasting for weeks, unintentional weight loss and white spots on the tongue or mouth During late-stage HIV infection, the risk of developing a life-threatening illness is much greater. Serious conditions may be controlled, avoided, and/or treated with other medications, alongside HIV treatment.
 HIV and AIDS myths and facts
HIV and AIDS myths and facts
There are many misconceptions about HIV and AIDS. The virus cannot be transmitted from shaking hands, hugging, casual kissing, sneezing, touching unbroken skin, using the same toilet, sharing towels, sharing cutlery, mouth-to-mouth resuscitation or other forms of casual contact.
Status of AIDS in India
India has the third largest HIV epidemic in the world. In 2016, HIV prevalence in India was an estimated 0.3%. This figure is small compared to most other middle- ncome countries but because of India’s huge population (1.324 billion) this equates to 2.1 million people living with HIV. In the same year, an estimated 62,000 people died from AIDS-related illnesses.
Overall, India’s HIV epidemic is slowing down, with a 32% decline in new HIV infections (80,000 in 2016), and a 54% decline in AIDS-related deaths between 2007 and 2015.
The HIV epidemic in India is driven by heterosexual sex, which accounted for 87% of new infections in 2015.However, the epidemic is concentrated among key affected populations such as sex workers. The vulnerabilities that drive the epidemic are different in different parts of the country. The three states with the highest HIV prevalence (Manipur, Mizoram, Nagaland) are in the east of the country. Some states in the north and northeast of the country have also reported rising HIV prevalence.
Among key affected populations, sex workers and men who have sex with men have experienced a recent decline in HIV prevalence.
Prevalence among people who inject drugs was previously stable but has been rising in recent years. Transgender people are also emerging as a group at high risk of HIV transmission, despite all four of these groups being prioritized in the Indian national AIDS response since its inception in 1992.
In 2016, HIV prevalence in India was an estimated 0.3%. This figure is small compared to most other middle-income countries but because of India’s huge population (1.324 billion) this equates to 2.1 million people living with HIV
 Sex workers and HIV
Sex workers and HIV
In 2016, an estimated 2.2% of female sex workers in India were living with HIV, although this figure varies between states.
For example, one 2013 study cited HIV prevalence among sex workers in Maharashtra at 17.9%, Manipur at 13.1%, Andhra Pradesh at 9.7% and Karnataka at 5.3%.Although sex work is not strictly illegal in India, associated activities such as running a brothel are.
This means authorities can justify police hostility and brothel raids. Stigma and discrimination against sex workers restrict their access to healthcare.
A 2011 study in Andhra Pradesh indicated a significant association between police abuse and increased risk of HIV transmission and inconsistent condom use. Sex workers are one of the high-risk groups targeted by India’s National AIDS Control Organization (NACO) with peer-to-peer HIV interventions (when individuals from key affected populations provide services to their peers or link them to services within healthcare settings). In 2015, NACO reported reaching 77.4% of sex workers with HIV prevention activities of this kind.
Male sex workers are particularly vulnerable to HIV. A study of men who have sex with men (sometimes referred to as MSM) who attended STI clinics at Mumbai and Hyderabad, two large cities in India, found that 70% of them engaged in sex work. Of those who engaged in sex work, HIV prevalence was found to be 43.6%, compared to 18.1% among all men who have sex with men attending the clinics.
Around 4.3% of men who have sex with men in India are living with HIV, with just over a third aware of their status. A 2015 study of men who have sex with men, conducted across 12 Indian cities, found that 7% tested positive for HIV. Just under a third (30%) of those who reported having anal or oral sex with a man in the past 12 months were married to a women and engaging in heterosexual sex.19. The study also found evidence of emerging epidemics among men who have sex with men in urban areas not previously recognised as having high HIV burdens.
The legal status of same-sex conduct in India has fluctuated in recent years. In December 2013, India’s Supreme Court re-criminalised adult consensual same-sex sexual conduct, after the Delhi High Court had decriminalised it in 2009. This raised fears about access to HIV prevention and treatment for men who have sex with men. However, in February 2016, India’s Supreme Court announced a review of the 2013 decision.
Male sex workers are particularly vulnerable to HIV. A study of men who have sex with men (sometimes referred to as MSM) who attended STI clinics at Mumbai and Hyderabad, two large cities in India, found that 70% of them engaged in sex work.
 People who inject drugs (PWID) and HIV
People who inject drugs (PWID) and HIV
The number of people who inject drugs (sometimes referred to as PWID) living with HIV in India is rising. The prevalence rate remained steady at around 7% between 2007 and 2013, but was estimated at 9.9% in 2015.
Injecting drug use is the major route of HIV transmission in India’s north-eastern states. HIV prevention efforts in the north-east have been effective in reducing the number of new infections. However, there is evidence that the number of people who inject drugs is growing.30
The same study found HIV prevalence to be three times higher for women who inject drugs than men who do so.
HIV prevention activities for people who inject drugs in India include needle and syringe exchanges and opioid substitution therapy (OST), with the former intervention more common. NACO reports the number of clean needles and syringes distributed as 16.5 million as of September 2015, a figure that is rising year on year.
OST was incorporated into the harm reduction programme in 2008. As of 2014, there were around 150 OST centres supporting nearly 18,000 people who inject drugs. Plans to increase the number of OST centres has been slow and coverage as of 2016 remains low, with only 213 OST centres nationwide.
Migrant workers and HIV
Research worldwide has linked migration to increases in HIV transmission. There are an estimated 7.2 million migrant workers in India, of whom 0.19% are living with HIV – much higher than the national prevalence of 0.26%.34.
 NACO categorises migrants as a ‘bridge population’, as they form a link between urban and rural areas, and between groups that are at high and low-risk of HIV transmission. HIV testing among this group remains low, standing at 11.32% in 2016.
NACO categorises migrants as a ‘bridge population’, as they form a link between urban and rural areas, and between groups that are at high and low-risk of HIV transmission. HIV testing among this group remains low, standing at 11.32% in 2016.
Despite being an important driver of the HIV epidemic in India, data on migrant sexual behaviour is limited. In 2014, UNAIDS reported that 75% of women testing positive in India have a husband who is a migrant labourer. Moreover, 0.9% of people who have migrated from a rural to an urban area are HIV-positive.
Key highlights of the HIV and AIDS (Prevention and Control) Bill, 2017 Prohibition of discrimination against
HIV positive persons: The Bill sets various grounds on which discrimination against HIV positive persons is prohibited. These include the denial, termination, discontinuation or unfair treatment with regard to employment, educational establishments, health care services, residing or renting property, among others.
Informed consent and disclosure of HIV status: The Bill requires that no HIV test, medical treatment, or research will be conducted on a person without his informed consent.
Role of the Union and State Governments: The Union and State Governments shall take measures to prevent the spread of HIV or AIDS, provide anti-retroviral therapy and infection management for persons with HIV or AIDS, facilitate their access to welfare schemes especially for women and children, and others.
Role of the Ombudsma n: An ombudsman shall be appointed by each state government to inquire into complaints related to the violation of the Act and the provision of health care services.
Guardianship: A person between the age of 12 to 18 years who has sufficient maturity in understanding and managing the affairs of his HIV or AIDS affected family shall be competent to act as a guardian of another sibling below 18 years of age.
Court proceedings: Cases relating to HIV positive persons shall be disposed off by the court on a priority basis. In any legal proceeding, if an HIV infected or affected person is a party, the court may pass orders that the proceedings be conducted (a) by suppressing the identity of the person, (b) in camera, and (c) to restrain any person from publishing information that discloses the identity of the applicant.

