Caring for the Aging Spine
With rapid developments in medical and surgical fields, spine ailments can be successfully managed using medications, injections or surgery. But healthy lifestyle and proper spine care are also necessary to prevent or mitigate spine complications in the elderly…
By Dr H S Chhabra
According to Population Census 2011, there are nearly 104 million elderly persons (aged 60 years or above) in India of which 53 million are females and 51 million males. A report released by the United Nations Population Fund and Help Age India suggests that the number of elderly persons is expected to grow to 173 million by 2026. It is expected to lead to greater challenges for medical care in terms of care delivery, cost, and maintaining quality of life for aging individuals.
 Orthopaedic surgeons shall face unique challenges in caring for this aging population. In particular, spine surgeons have to face the challenges of treating the growing numbers of patients with traumatic or insufficiency spine fractures as well as degenerative deformities and instabilities. The goal of the surgeon should be to enable the elderly to perform their usual activities of daily living independently or with minimal dependence on the family or care takers.
Orthopaedic surgeons shall face unique challenges in caring for this aging population. In particular, spine surgeons have to face the challenges of treating the growing numbers of patients with traumatic or insufficiency spine fractures as well as degenerative deformities and instabilities. The goal of the surgeon should be to enable the elderly to perform their usual activities of daily living independently or with minimal dependence on the family or care takers.
Attention must be given to each aspect and probable degenerative condition of aging in order to assist the aging population in this goal. Care of the aging spine and pain management are some areas where particular focus has to be given.
Significant degeneration of the spine begins in the third decade of life, eventually leading to progressive disc height loss and ligamentous/capsular hypertrophy, or thickening. As degeneration progresses, bony and soft tissue failure can develop, leading to a variety of spinal conditions.
What are the most common spine conditions affecting the elderly?
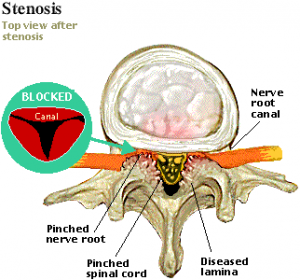
In older adults who have isolated low back and/or neck pain, more than half are due to degenerative facet joint arthritis. This is a type of osteoarthritis that affects the parallel column of joints that connect the individual vertebra of the spine behind the spinal canal. Other common causes of back/neck pain are also largely a result of the aging process, with degenerative spine changes including spinal stenosis (narrowing of the central tube housing the spinal cord and spinal nerves), spondylolisthesis (misalignment of one vertebra over another), and/or neural foraminal stenosis (narrowing of the tunnels where the spinal nerves exit the spine). In spinal stenosis, the typical symptom is claudication in which the individual has pain in the leg which increases as the individual walks and ultimately needs to sit or lie down to relieve the pain. This distance gradually reduces with time and can cause major disability. Any or all of these conditions can cause pain, which may also radiate to the arms or legs due to irritation or compression of the spinal nerves.
Genetics and family history, obesity, smoking, certain occupations (excessive driving, lifting, or sitting in front of a computer), or a history of previous trauma are also reasons for the acceleration of the degenerative process.
There are other common causes of back pain in the elderly. Sudden, sharp back pain can be a result of a vertebral compression fracture, especially in those who have advanced osteoporosis.
 Osteoporosis is a large problem for the growing population of older adults as it leads to decreased bone strength and, thus, bone fractures including spinal fractures. After reaching a peak between the ages of 16-25 years, bone mass slowly but continuously decreases at a rate of 0.5% per year in women and 0.3% per year in men. By the time they reach the age of 60, elderly men would have lost ~30% and elderly women ~50% of their total bone mineral density. It is estimated that as many as 61 million Indians have osteoporosis and approximately 80% of the urban Indian population is vitamin D deficient. Fractures can be the first sign of weak bones from osteoporosis. According to one report, vertebral fractures are present in about 25% of postmenopausal women, with rates increasing dramatically with age.
Osteoporosis is a large problem for the growing population of older adults as it leads to decreased bone strength and, thus, bone fractures including spinal fractures. After reaching a peak between the ages of 16-25 years, bone mass slowly but continuously decreases at a rate of 0.5% per year in women and 0.3% per year in men. By the time they reach the age of 60, elderly men would have lost ~30% and elderly women ~50% of their total bone mineral density. It is estimated that as many as 61 million Indians have osteoporosis and approximately 80% of the urban Indian population is vitamin D deficient. Fractures can be the first sign of weak bones from osteoporosis. According to one report, vertebral fractures are present in about 25% of postmenopausal women, with rates increasing dramatically with age.
Another less common cause can be a spinal tumour, whether primary or metastatic. Infection, especially if the patient has recently had a spine procedure, is another possible condition that necessitates prompt diagnosis and treatment.
These conditions can be diagnosed and evaluated with x-rays and magnetic resonance imaging, and PET scan if required.
How can these conditions be treated?
The treatment for degenerative changes of the spine leading to pain starts with lifestyle and ergonomic adjustments such as sleep positions, appropriate desk and chair height, and proper lifting technique. Then anti-inflammatory medications and physical therapy are utilized. Neurotropic medications may be required for claudication symptoms. The next steps include interventional pain management techniques, such as facet joint nerve blocks for facet arthritis or epidural steroid injections for sciatic-like pain.
 The majority of patients will have tolerable pain after a series of these conservative treatments, but some may require surgery for relief. Most conditions can be treated with same-day, minimally invasive surgery, although some may require much more extensive surgery. Certain conditions, such as spinal stenosis or sciatic-like pain (radiculopathy), are more easily treated with surgery, while others, such as facet osteoarthritis, are not.
The majority of patients will have tolerable pain after a series of these conservative treatments, but some may require surgery for relief. Most conditions can be treated with same-day, minimally invasive surgery, although some may require much more extensive surgery. Certain conditions, such as spinal stenosis or sciatic-like pain (radiculopathy), are more easily treated with surgery, while others, such as facet osteoarthritis, are not.
Vertebral compression fractures can most often be treated conservatively. This involves management of the pain and management of osteoporosis. Osteoporosis management involves pharmacological management (generally oral or intravenous bisphosphonates or denosumab injection and teriparatide injections for severe osteoporosis), calcium supplementation, general conditioning exercises like walks and dietary/fall prevention counselling. If pain doesn’t respond or if there are signs of spinal cord/nerve compression, surgery may be required. Kyphoplasty is a minimally invasive, same-day procedure where cement is injected into the fractured vertebral body, which, in almost all cases, relieves pain and stabilizes the bone from further collapse (avoiding the dangerous “hunchback” shape of the spine). In case of instability or nerve/spinal cord deficit, stabilization with pedicle screws along with decompression by removal of pressure from nerves/spinal cord may be required. In severe osteoporosis, cement augmentation may be required for stable pedicle screw fixation.
Spinal tumours, whether primary or metastatic, need to be evaluated by an oncologist as soon as they are detected. Standard interventional pain management techniques may help with the pain symptoms, but treatment using a complement of chemotherapy, radiation, and surgery will likely be recommended to address the tumours directly.
Infection of the spine, if not treated promptly, can lead to the obliteration of the spinal canal or nerves and/or septic shock. Fortunately, an extensive course of antibiotics and removal of spinal hardware (if applicable) are able to treat most infections.
The age of the patient is not a contraindication for spine surgery. The benefits of spine surgery for older patients, including less-invasive operations, outweigh the risks associated with those procedures wherever it is indicated. Also, spine surgery has seen rapid advancements in operative techniques, implants and biologics, and equipment such as computer assisted navigation and surgical robotics increasing the safety and accuracy of surgery.
What conditions can complicate the treatment?
Other conditions involving the spine can accelerate the development or complicate the treatment of these conditions. Some of these include ankylosing spondylitis, idiopathic scoliosis, rheumatoid arthritis, previous spine surgery, and cancer.
Medical conditions unrelated to the spine can also complicate treatment. Osteoporosis, for example, can cause or accelerate many of the above conditions, so proper treatment through a primary care provider or endocrinologist can help prevent progression of these conditions. Obesity also makes treatment of these conditions difficult, so proper dieting and appropriate exercise can help immensely. Smoking is well known to exacerbate all pain syndromes, so cessation is highly recommended.
How can we reduce the incidence of spine conditions?
Ergonomics at home and work are extremely important and go a long way in helping to prevent or reduce back or neck aches. When sitting at a computer desk, avoid slouching of the back and stooping of the neck. Make efforts to raise the computer monitor to eye level and adjust seat height to facilitate optimal positioning. When lifting heavy objects, be sure to bend at the knees and not at the waist, and push rather than pull as much as possible.
Proper sleep bedding and positions are important as well. A firm mattress and a pillow that allows your neck to lie in a neutral position are very important for neck and back stability. Also, sleeping with a pillow under the knees when lying supine or with a pillow between the knees when on the side can help reduce stress on the lower back.
Walking alone can improve flexibility, strength, and blood flow to the spine and intervertebral discs, which can help prevent injury. A morning or evening walk for 45 minutes can easily be incorporated into a daily routine, before or after meals. For those whose mobility is limited, staying out of bed as much as possible is the main priority.
 A strong core is essential to preventing spine injury, so static exercises that strengthen and tone the abdominal, lower back, and neck muscles are also effective. Yoga and pilates (within reasonable limits) can also be helpful in creating and maintaining flexibility and strength of the spine and core.
A strong core is essential to preventing spine injury, so static exercises that strengthen and tone the abdominal, lower back, and neck muscles are also effective. Yoga and pilates (within reasonable limits) can also be helpful in creating and maintaining flexibility and strength of the spine and core.
Thanks to smartphones and mobile apps, our lives have become much easier. Mobile health is emerging as the most convenient way to deliver services remotely, and collect outcomes in real-time, thus contributing to disease management by transferring care from hospital to home. Nowadays, there are mobile apps like Snapcare which are meant to help people with back pain and to teach them self-care of the back.
Globally, there have been rapid developments in prevention, diagnosis and comprehensive management of various spinal ailments in both medical and surgical fields. Prompt diagnoses such as vertebral fractures and infections can significantly reduce pain and even save lives. Older adults with sudden severe back pain and/or fever should be taken to urgent or emergent care as soon as possible. Timely intervention is crucial in better and efficient management of spine-related conditions affecting the elderly.
To summarize, prevention is better than cure. Healthy lifestyle and spine care are necessary to escape the agony of spine problems. Early diagnosis and timely intervention is necessary to prevent complications in the management of spine conditions. With advancements in management of spine ailments, they can be successfully managed using medications, injections or surgery. Spine surgery is safe in the elderly and can give excellent results in expert hands.
(The author is Chief of Spine Service and Medical Director, Indian Spinal Injuries Centre, New Delhi)

