Eliminating the scourge
Successful global implementation of HPV vaccination and effective screening strategies offer the hope for eventually eradicating cervical cancer. It’s the need of the hour to address myths related to the HPV vaccine…
By Dr Shruti Bhatia

Cervical cancer is the second most common type of cancer found in women worldwide. In developing countries including India, it is the most common cancer causing death in women.
 Every year 1,22,800 new cases of cervical cancer are diagnosed in India and almost half of them die from the disease. Human papilloma virus (HPV) is a well- established causative agent of cervical cancer. HPV are a group of more than 100 related viruses. Persistent infection with high risk strains such as 16,18 are responsible for cervical cancer cases worldwide. HPV is also associated with genital warts, cancers of vulva, vagina, anus, penis, and oropharynx.
Every year 1,22,800 new cases of cervical cancer are diagnosed in India and almost half of them die from the disease. Human papilloma virus (HPV) is a well- established causative agent of cervical cancer. HPV are a group of more than 100 related viruses. Persistent infection with high risk strains such as 16,18 are responsible for cervical cancer cases worldwide. HPV is also associated with genital warts, cancers of vulva, vagina, anus, penis, and oropharynx.
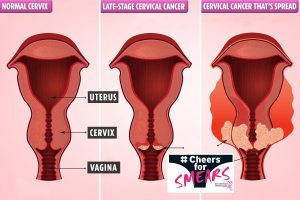
More than 80% of HPV related cervical cancers can be prevented with vaccinations if given before a girl or woman is exposed to the virus in cervix – the lower part of the uterus that connects to the vagina. Vaccination and routine screening are necessary to prevent and eradicate the disease. Three vaccines have been approved worldwide:
Cervarix: This bivalent vaccine targets HPV types 16 and 18.
Gardasil: It is a quadrivalent vaccine as it targets HPV types 16,18 as well as 6 and 11, so not only providing prevention against cancers but also genital warts.
 Gardasil 9: This vaccine targets HPV types 6,11,16 and 18 along with 31,33,45,52,58 which are responsible for 90% cases of cervical cancer and most of the genital warts. Currently, Gardasil 9 is not available in India.
Gardasil 9: This vaccine targets HPV types 6,11,16 and 18 along with 31,33,45,52,58 which are responsible for 90% cases of cervical cancer and most of the genital warts. Currently, Gardasil 9 is not available in India.
In females, HPV vaccination is recommended at age 11 or 12, but it can be given as early as age 9. Catch up vaccination is permitted upto the age of 45 years. In girls younger than 15, a 2-dose schedule is recommended. Three-dose schedule is necessary in females between ages 15 and 45. There is no need of any booster dose as the benefit lasts for a long time. Currently, vaccine is not recommended for pregnant woman, although a pregnancy test is not required before vaccination. If pregnancy occurs, it is recommended that reminder of the series is deferred until after delivery. Immunocompromised patients should follow a three-dose schedule irrespective of age when vaccination was initiated. Females who have been vaccinated should still have their screening through cytology or HPV testing.
 Vaccination rates are currently low as it touches issues related to adolescent sexuality, parental barriers due to lack of knowledge and perceived need for vaccination and cost. Successful global implementation of HPV vaccination and effective screening strategies offer the hope for eventually eradicating cervical cancer. Hence, it’s the need of the hour to address myths related to the HPV vaccine and help everyone understand that vaccine is safe with no side effects.
Vaccination rates are currently low as it touches issues related to adolescent sexuality, parental barriers due to lack of knowledge and perceived need for vaccination and cost. Successful global implementation of HPV vaccination and effective screening strategies offer the hope for eventually eradicating cervical cancer. Hence, it’s the need of the hour to address myths related to the HPV vaccine and help everyone understand that vaccine is safe with no side effects.
(The author is Senior Consultant, Dept. of Gynae Oncology, Sri Balaji Action Cancer Hospital, New Delhi)

