Innovations in Healthcare
Current Covid-19 pandemic has been a problem that has engulfed the entire globe. Healthcare delivery has been impacted in ways that are hard to even imagine…..
By Dr Vijay Agarwal
Necessity is the mother of invention” is a well- known proverb meaning that a problem encourages creative efforts to solve the problem. Specialists and super specialists who were against using telemedicine have embraced the same and enjoying the same. A lot of enterprising persons in the community developed innovative solutions to solve some aspect of this elephantine problem. The healthcare providers have also contributed immensely by innovations to tackle some unique problems.
Consortium of Accredited Healthcare Organizations (CAHO) decided to hold a one-day virtual program to provide a platform where these innovations can be presented and the best ones can be awarded. 55 hospitals submitted the brief of their innovations. Seven-member jury shortlisted 18 of these and then a winner, 2 runners-up and 2 encouragement awardees were chosen.
We are presenting here these best 5 innovations –
1. Aravind Eye Hospital (Winner)


Problem Statement:
Slit lamp examination is an important part of eye check-up.Ophthalmologists cannot achieve social distancing during slit lamp examination of patients during which patient and doctor are at close proximity. When trying to examine the eyes their gloved hands may also get contaminated with tears which can be infective and the hot breath gets directed upwards because of the masks worn by patients which cause fogging of the 90D lens within seconds making examination of the fundus very difficult.
Solution:
Though protective shields of various dimensions and material are available they are very small and only serve as a barrier and does not protect fully. In order to design a slitlamp shield of appropriate size we first determined the potential distance of aerosol spread by simulating a patient’s cough using a nozzle spray with fluorescent dye, experiments with smaller size shield showed that the droplet crossed the shield and reach the examiner, hence they give a false sense of security and are inadequate and don’t serve the purpose.
Depending on the amount of aerosol spread we have designed a safe, user friendly and an ergonomical slitlamp shield which gives complete protection from aerosol without hindering our hands during examination of patients in the slit lamp. We have also used stickers in the shield to help in fixation of the patients during examination. The ease to disinfect between every patient, transparency allowing easy intervention and communication, user friendliness to enable to perform manoeuvres and ergonomic suitability make it an ideal “Guardian of the slitlamp” for safe slitlamp examination.
While we start to examine a patient, we spend significant time to get the complains and the history of the patient that increases the risk of exposure to aerosol generated while talking which in turn increases the risk of contracting Covid-19. We have started to practise “History over phone” where the doctor or the ophthalmic assistant call the patient over phone after registration and gets their history and complaints and fills them up in the Electronic Medical Record (EMR) so when the patient comes to the doctor for examination the complaints and history is already entered and we can start examination. This system is very simple and not only received well by the doctors but also by the patient as their exposure is also reduced. This system reduces the amount of time spent with the patient at close proximity by 50%.
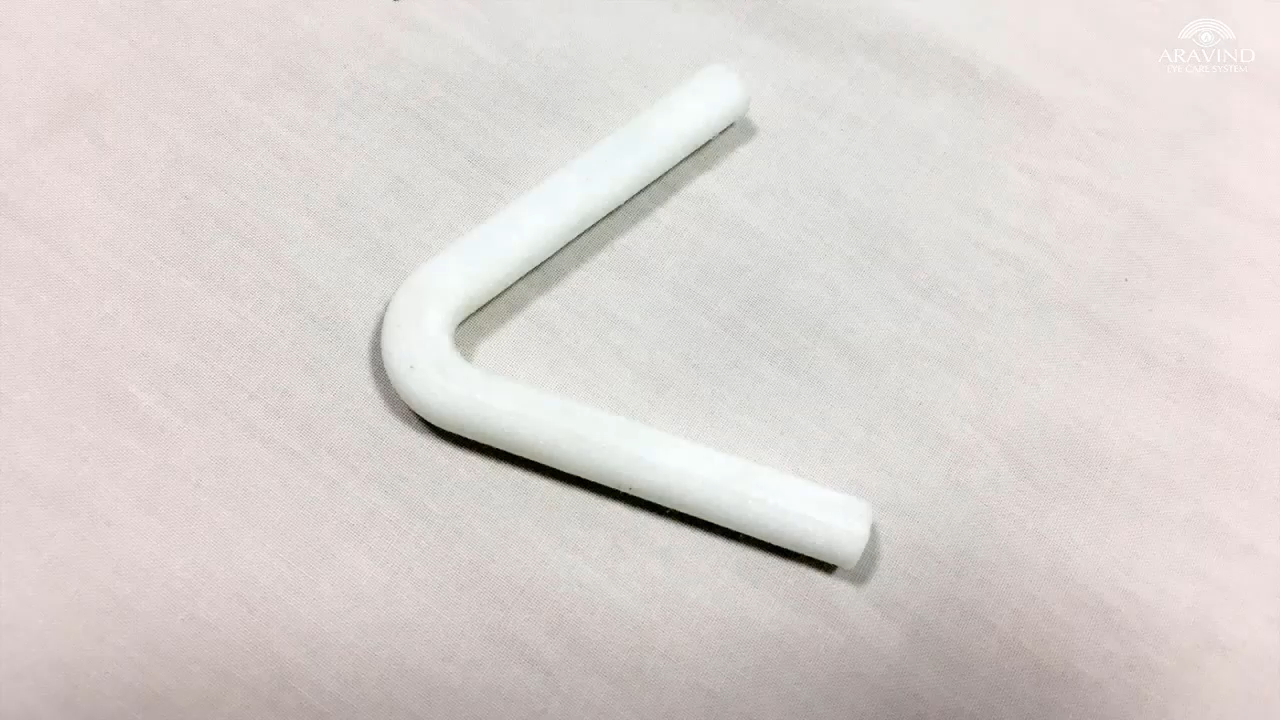
Many a times the patient closes their eyes when we use bright light to examine their eyes during slitlamp examination. This leads the ophthalmologist to use their hands to retract the eyelids and during Covid pandemic there is a high risk of contamination of the hands with tears or accidental touching of the mask while doing so. We have designed and 3D printed a novel “I-opener” which is a simple, cost effective and patient friendly ‘V’ shaped device.
Ophthalmologist use a 90D lens to examine the fundus in all the patient, due to Covid-19 all patients are made to wear a 3 PLY mask. This new normal has led to the hot breath of the patient to be directed upwards. This air causes fogging of the 90D lens within seconds during examination and produces a blurred image so we will not be able to see the fundus. As the breath of the patient is also infective, we need to clean the lens between each patient with sanitiser and this also removes the coating of the 90D lens and damages it.
2. Caritas Hospital (Runners- Up)


Problem Statement:
During Covid-19, healthcare workers were at high risk while caring for Covid-19 suspected or confirmed patients. The healthcare personnel who intubate with the patient also were at high risk because of the aerosols generated during the procedure.
Solution:
The innovative team of Caritas Hospital led by Caritas Heart Institute has come with a Cost effective “Video Laryngoscope”. The ultimate aim behind the idea is to make a laryngoscope at an affordable cost. Dr.Nice Varghese, Resident Medical Officer of Caritas Heart Institute has developed a video laryngoscope in consultation with the consultants in Cardiology, Cardiothoracic surgery, Cardiac Anaesthesia, Pulmonology, Microbiology etc.
The final cost for this laryngoscope will be around Rs. 5000/- only. The hospital management has given full support to the team in this innovation and the product has come out very effective, especially during this Covid-19 era.
The chances of getting COVID-19 infection while intubating a patient can be avoided using this equipment.
3. SreeRenga Hospital (Runners- Up)

Problem Statement:
The global shortage of quality PPE such as N95 face masks during the Covid-19 pandemic led to rapid cost escalation for high quality products and the entry of sub-par and spurious products which compromised the safety of both patients and the health care workers.
Solution:
While none can contest the superiority of manufacturer-delivered N95 face masks, presented herein is an evidence-based approach to safely decontaminate and re-use an N-95 mask multiple times, without any significant loss of efficiency.
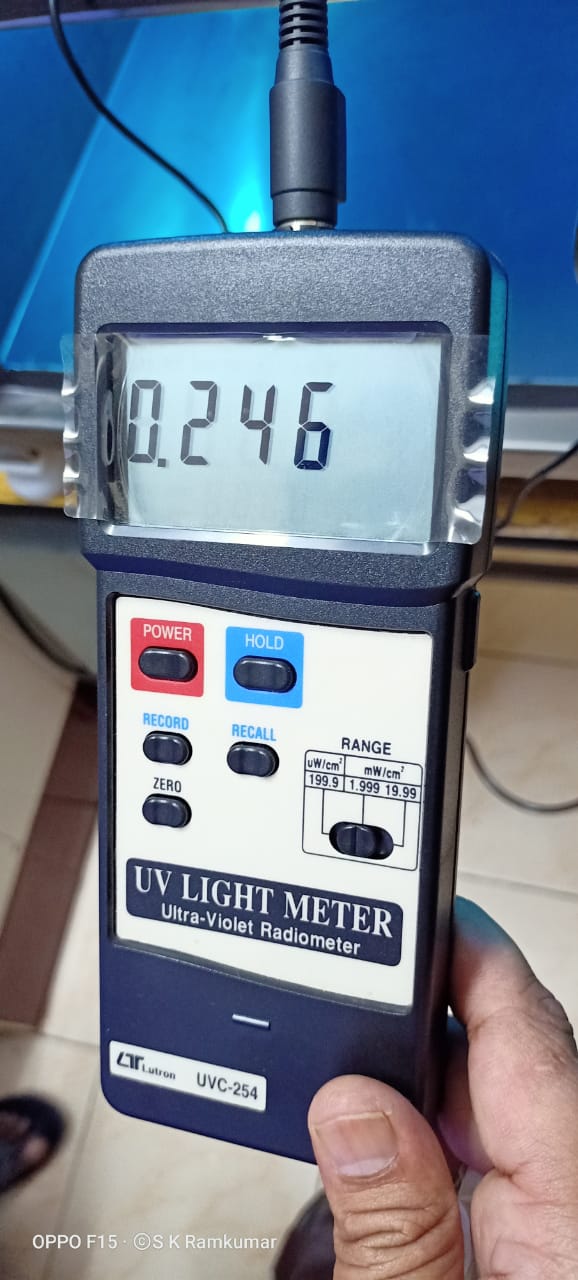
Decontamination and re-use of high quality N95 masks seemed imperative, to provide quality care at lower costs. Among the various modalities to implement the re-use of N95 masks, the Ultraviolet Germicidal Irradiation (UVGI) approach is attractive to hospital settings, owing to its relative ease of setting up, operation and process efficiency.
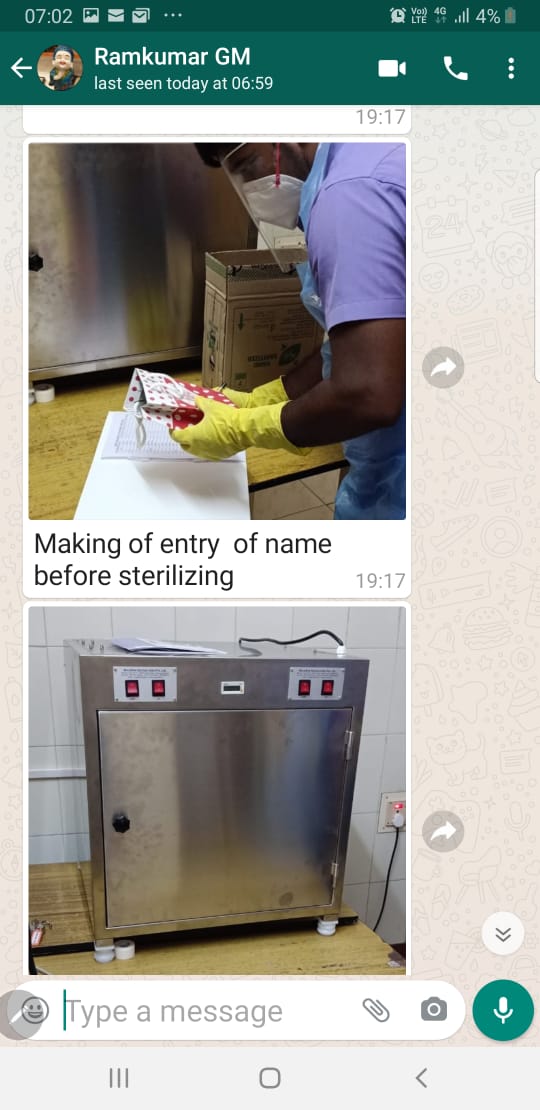
Enthused by the validated model (University of Nebraska Medical Centre, USA) of using UVGI to safely decontaminate and re-use an N95 mask multiple times before discarding it, Sree Renga Hospital, Chengalpattu, Tamil Nadu has designed a decontamination chamber fitted with UV lamps, defined a process flow to disinfect used N95 masks and trained technicians of the Central Sterile Supply Department (CSSD) to safely decontaminate and distribute the sterile N95 masks over multiple cycles of decontamination.
Challenge was to get the validation of protocol and certification of the product. Germicidal UV, also known as UV-C, is typically generated with mercury-based lamps that operate at 254 nm. Light at this wavelength is relatively strongly absorbed by nucleic acids, resulting in damage to RNA and DNA molecules in pathogens, which prevents their function or reproduction.
In literature, extensive decontamination and durability studies have been performed on 15 models of N95 face masks to evaluate how well Ultraviolet Germicidal Irradiation (UVGI) using UV-C bulbs (254 nm) decontaminates influenza virus and affects strap, filtration component, filtration performance and fit, pressure drop, fluid resistance and flammability characteristics. Based on the results of these studies, two ASTM consensus standards describing how to evaluate and optimize UVGI decontamination on N95 face masks for threat agents of interest have also been developed. UVGI was shown to be effective (3 mean log reduction) for the facemask material of N95 models including the straps
The UVGI protocol was tested on three different microorganisms (E.Coli ATCC 25922, Pseudomonas aeruginosa ATCC
27853, Spores (Bacillus stearothermophilus), each for three different time durations (15 mins, 43 mins and 60 mins) – contained either in a sample disc while being subjected to UVGI or having been injected into the inner or outer surface of an N95 mask.
Evaluation of the presence of the microorganisms after UVGI showed a log 5 reduction (complete absence) after UVGI of 1J/cm2.
The tests were conducted at NABL-accredited Anderson Diagnostic Services Pvt Ltd, Chennai.
4. Meenakshi Hospital (Encouragement Award)


PROBLEM STATEMENT:
Covid-19 spreads between people through direct, indirect (through contaminated objects or surfaces), or close contact with infected people. People who are in close contact (within 1 metre) with an infected person can catch COVID-19 easily. Healthcare workers like doctors, nurses and other direct patient care staffs are more prone to this deadly virus.
Solution:
To avoid the close contact in major areas, our hospital has come up with very useful and ahead of one’s time innovation known as “MOBILEPAIRED BLUETOOTH STETHOSCOPE “which aids the consultants and physicians to conquer this Covid situation.
The main aim of the mobile Bluetooth stethoscope is to avoid close contact between patients and doctors for longer period during this Covid period. It also focuses on hearing the sound from anywhere in the world without time frame and limits.
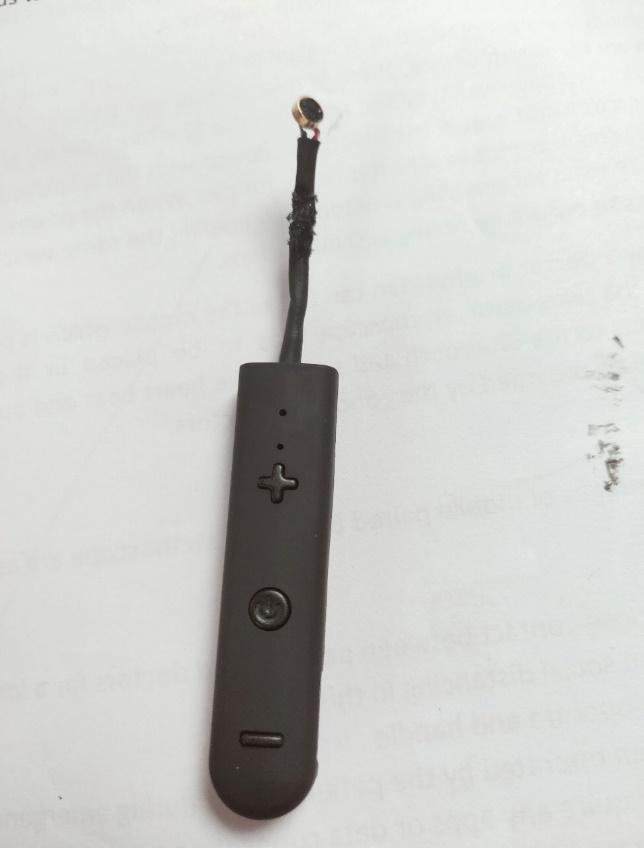
Our mobile paired Bluetooth stethoscope is 15 cm long and has acoustic stethoscope – based chest piece, amplification tube with Bluetooth recording options in it with a light indicator. It consists of power on/off switch, volume control switches.
In this technology a simple method of replacements in techniques with the device parts is used as principle. In every Bluetooth device, there is a microphone and speaker which allows us to acquire and hear the acoustics, we have removed the mic from the Bluetooth device and placed it inside the chest piece of a stethoscope and sealed the Bluetooth device with the stethoscope. Now we can pair the Bluetooth device using our mobile which is ready for use. When the power on switch is enabled, the same switch can be used for enabling Bluetooth by holding the same switch. Once the Bluetooth in the stethoscope is on, we can ensure by seeing LED indications.
Now a doctor or physician can call to the mobile which is paired with the Bluetooth stethoscope, now the Bluetooth stethoscope has to be placed in the patient’s chest which automatically connects to the Bluetooth and sounds like heart beat and auscultation can be clearly observed and can also be recorded by the concerned doctors.
The mobile paired Bluetooth technology works in a simple principle which is not only used in isolation areas but the applications to the devices are many. The successful measured outcomes in our hospital are listed below :
• This device is abundantly used in COVID areas, COVID ICUS and screening OPDs. If a patient is suspected, this device is also used in Out-patient consultation areas to maintain distance and to avoid getting infections.
• Our hospital is the first hospital in delta region to develop virtual ICU with all facilities.For critical care consultants in virtual ICU, this mobile paired Bluetooth stethoscope provides a major comfort and ease in diagnosing and providing care.
• During teleconsultation by the doctors from anywhere to the hospital, provides a better quality of care.
• It provides a better and safer work place environment and provides satisfaction to doctors and health care workers.
• There is no distance limit for contacting the patients and observing the sounds which is very helpful for the doctors in all times.
5. Nanavati Super Speciality Hospital (Encouragement Award)


Problem Statement
1. Timely reporting to health authorities w.r.t RT PCR test results.
2. Delayed action on test orders given by Consultant ranging to more than 4 hours.
3. No method of monitoring the event in real-time when Consultant has ordered investigation and status of sample and report.
4. Non-availability of reports status for patients requiring urgent intensive care, waiting in Accident & Emergency and consultant review.
5. Absence of real-time monitoring resulting in the delayed intervention of lab administrators, which resulted in RT-PCR report turnaround time upward of 35 hours for outpatients and 36 hours for inpatients.
Solution
The implementation of Experience flow operations BOTs enabled AI-driven software had three components:
a) Non-Intrusive lab process decision-making application, through which users can view and track, prioritize the progress of each patient’s sample per: wards, speciality, ICU, or department-wise.
b) Real-time doctor intervention interface, through which a doctor can view real-time the status or progress of diagnostics of a patient’s sample through his smartphone; independent of his physical presence in the hospital. Doctors can also suggest history review for critical or abnormal sample results.
c) Self-guiding real-time patient experience application, through which a patient can track his laboratory investigation order’s status in the Experience Flow application.
A. Implementation of non-intrusive laboratory process monitoring application:
i. IT department along with the line staff and Experience Flow Team had mapped AS-IS process for each event, as per the quality standards defined by the National Accreditation Board Lab for Hospital (NABL) – under Quality Council of India.signed-off by Heads of Departments.
ii. Each subprocess was statistically modelled before the implementation of the AI-enabled application, with parameters such as specification limits and alerts for crossing thresholds defined as Red (outlier), Orange (delayed) and Green (within limits) to all the Covid -19 and non- Covid -19 wards etc.
iii. Standardization of email and report formats for various Departments and based on a variety of selection criteria as per speciality, doctor specific, ward-wise, department-wise, time range-wise, day-wise, month-wise, and test-wise all improved efficiencies and effectiveness of the lab process.
B. Implementation of lab doctor, administrator intervention interface application:
i. A doctor, administrator intervention interface application was additionally developed through which a Consultant can view the list of patient orders generated and collection status of investigations ordered by him as well as prioritizes the sample testing for a particular patient, in the mobile application.
ii. Lab administrator & quality team has access to view the AI bot-driven lab process progress of the patients.
C. Self-guiding real-time patient experience application:
i. After conducting through validation exercises to ensure the correctness of data captured in the Operations BOTs application from the LIS, the entire digital lab process was stabilized and monitored for compliance, by all users and stakeholders.
ii. The patient experience application was implemented to provide real-time tracking of the status of their lab order and collect feedback associated with each step of the journey.
5. Nanavati Super Speciality Hospital (Encouragement Award)
Problem Statement
1. Timely reporting to health authorities w.r.t RT PCR test results.
2. Delayed action on test orders given by Consultant ranging to more than 4 hours.
3. No method of monitoring the event in real-time when Consultant has ordered investigation and status of sample and report.
4. Non-availability of reports status for patients requiring urgent intensive care, waiting in Accident & Emergency and consultant review.
5. Absence of real-time monitoring resulting in the delayed intervention of lab administrators, which resulted in RT-PCR report turnaround time upward of 35 hours for outpatients and 36 hours for inpatients.
Solution
The implementation of Experience flow operations BOTs enabled AI-driven software had three components:
a) Non-Intrusive lab process decision-making application, through which users can view and track, prioritize the progress of each patient’s sample per: wards, speciality, ICU, or department-wise.
b) Real-time doctor intervention interface, through which a doctor can view real-time the status or progress of diagnostics of a patient’s sample through his smartphone; independent of his physical presence in the hospital. Doctors can also suggest history review for critical or abnormal sample results.
c) wwSelf-guiding real-time patient experience application, through which a patient can track his laboratory investigation order’s status in the Experience Flow application.
A. Implementation of non-intrusive laboratory process monitoring application:
i. IT department along with the line staff and ExperienceFlow Team had mapped AS-IS process for each event, as per the quality standards defined by the National Accreditation Board Lab for Hospital (NABL) – under Quality Council of India. signed-off by Heads of Departments.
ii. Each subprocess was statistically modelled before the implementation of the AI-enabled application, with parameters such as specification limits and alerts for crossing thresholds defined as Red (outlier), Orange (delayed) and Green (within limits) to all the COVID-19 and non-COVID-19 wards etc.
iii. Standardization of email and report formats for various Departments and based on a variety of selection criteria as per speciality, doctor specific, ward-wise, department-wise, time range-wise, day-wise, month-wise, and test-wise all improved efficiencies and effectiveness of the lab process.
B. Implementation of lab doctor, administrator intervention interface application:
i. A doctor, administrator intervention interface application was additionally developed through which a Consultant can view the list of patient orders generated and collection status of investigations ordered by him as well as prioritize the sample testing for a particular patient, in the mobile application.
ii. Lab administrator & quality team has access to view the AI bot-driven lab process progress of the patients.
C. Self-guiding real-time patient experience application:
i. After conducting through validation exercises to ensure the correctness of data captured in the Operations BOTs application from the LIS, the entire digital lab process was stabilized and monitored for compliance, by all users and stakeholders.
ii. The patient experience application was implemented to provide real-time tracking of the status of their lab order and collect feedback associated with each step of the journey.
Outcomes
Key deliverables of the automated laboratory process monitoring application:
a) Implementation of ExperienceFlow Operations BOTs enabled lab process monitoring application has resulted in a drastic improvement in terms of the average turnaround time (36 hours, 52 minutes before vs. 13 hours, 32 minutes after Experience Flow implementation) from the sample collection to report finalized of patients.
b) This data-driven approach with MIS reports for all stakeholders, a “WOW” step to the lab’s performance measurement, has changed the culture of the lab teams. The use of the digital platform saves several hundreds of manhours and provides a single version of truth for process performance review.
c) Average process turnaround time and patient wait time of lab reports reduced considerably, freeing machine & staff capacity. Consultants, as well as the hospital’s operations team now have access to real-time, patient wise, test-wise, speciality-wise status of the patient samples and reports, so that the medication to patients can be prioritized at the earliest. Employee performance is now tracked objectively to assess their specific training needs. Timely availability of precise information in the automated reports has helped senior management to take strategic decisions to improve the laboratory process performance.
(The author is President, Consortium of Accredited Healthcare Organizations (CAHO)

