Obstructed Flow
It is important to explore the best treatment option for aneurysm, an excessive localized enlargement of arteries such as those supplying blood to the brain. Aneurysm may remain silent or rupture, causing serious problems and even death
By Dr Rupinder Singh Baweja
An aneurysm is an excessive localized enlargement of an artery caused by weakness in the arterial wall. It can occur in important arteries such as those supplying blood to the brain, and the aorta; the large artery that originates at the left ventricle of the heart and passes down through the chest and abdominal cavities. The pathophysiology of an aneurysm (how it develops) is straightforward, although the causes are less well understood.
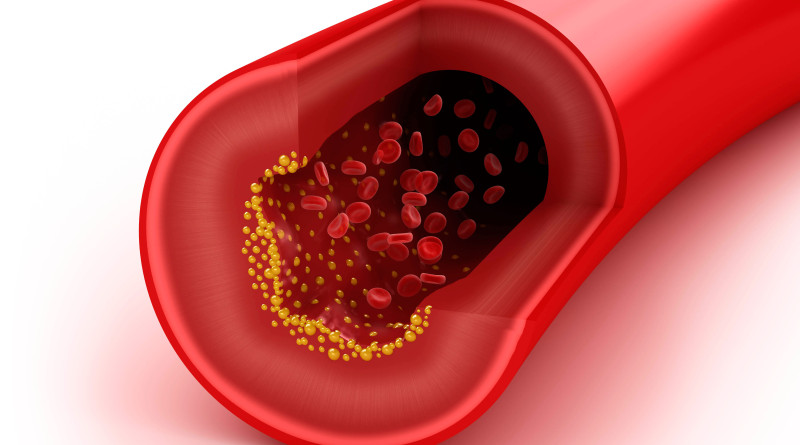
Most aneurysms do not themselves cause any symptoms. Even if an aneurysm does not rupture, however, a large aneurysm may obstruct circulation to other tissues. An aneurysm can also contribute to the formation of blood clots that obstruct smaller blood vessels, potentially causing ischemic stroke or other serious problems. If an aneurysm has remained undetected, the first sign of it could be when there is a complication – in particular, a rupture – with symptoms resulting from this rather than the aneurysm itself.
A number of risk factors are known to be associated with the development of aneurysms, and the same factors also affect the chances of a developed aneurysm then rupturing. However, it is not fully understood why the artery wall weakens in the way that it does to cause an aneurysm. Some aneurysms, though less common, are present as an artery defect at birth (congenital).
The majority of people living with an aneurysm do not suffer any of the complications like severe chest and/or back pain leads to heart attack and headache. However, managing the risk factors is important, because all of these possibilities are serious. If a brain aneurysm leads to subarachnoid hemorrhage (a kind of stroke), the main symptom is sudden extreme headache, often so severe that it is unlike any previous experience of head pain. Other symptoms of aneurysm rupture include pain, low blood pressure, a rapid heart rate, and light-headedness.
Endovascular coiling is a minimally invasive technique, which means an incision in the skull is not required to treat the brain aneurysm. Rather, a catheter is used to reach the aneurysm in the brain. During endovascular coiling, a catheter is passed through the groin up into the artery containing the aneurysm. Not all aneurysms need to be treated and your physician may choose to closely observe your aneurysm. There are two main treatment options for patients who need to have their aneurysm treated: Open surgical clipping and Endovascular therapy coiling. The open surgical clipping is performed by a neurosurgeon who will make an incision in the skin over the head, make an opening in the bone and dissect through the spaces of the brain to place a clip across the aneurysm where it arises from the blood vessel. This prevents the blood flow from entering the aneurysm. Most elective patients spend 2-3 nights in the hospital and then will go home on light restricted activity for 1-2 months after surgery.
There have been considerable advances in open surgery techniques. Many neurosurgeons can now perform mini craniotomies, or eye brow incisions to clip an aneurysm. In some patients, a small incision is made over the eyebrow. A small two inch window is then made in the bone over the eye and through this incision a small clip is placed across the opening of the aneurysm. These patients usually spend 1-2 days in the hospital after surgery and then go home. Patients are usually on light restricted activity for 1-2 months after surgery. However, it is still an invasive procedure and takes longer to recover from than a coiling procedure.
Endovascular treatment is performed by a neuro interventional surgeon who may be a neuro radiologist, neurosurgeon, or neurologist that has completed additional training. Studies have shown that patients with a ruptured aneurysm tend to do better in the long term after a coiling procedure.
A coiling procedure is performed as an extension of the angiogram. A catheter is inserted into a vessel over the hip and other catheters are navigated through the blood vessels to the vessels of the brain and into the aneurysm. Coils are then packed into the aneurysm up to the point where it arises from the blood vessel, preventing blood flow from entering the aneurysm. Most patients will go home the next day after surgery and are back to normal activities the following day. More than 125,000 patients worldwide have been treated with detachable platinum coils
Additional devices, such as a stent or a balloon, may be needed to help keep the coils in place inside the aneurysm. Stent assisted coiling involves permanently placing a stent in the vessel adjacent to the aneurysm to provide a scaffolding of support that keeps the coils within the aneurysm sac. Balloon remodeling involves temporarily placing a removable balloon adjacent to the aneurysm while coils are positioned in the aneurysm.
There have been considerable advances in endovascular techniques over the last few years and the field continues to evolve. Most notable is the use of new flow diverting embolization devices. These devices are similar to a stent in that they are placed into the main vessel adjacent to an aneurysm. These devices divert flow away from the aneurysm and provide scaffolding for healing of the vessel wall to occur. Over time, the aneurysm disappears.
Such technology allows doctors to treat many aneurysms that were previously considered untreatable or that were considered to be high risk by other methods. There are many other new devices that are becoming available as well, such as newer that are easier and safer to deliver, as well as stents that can bridge two vessels.
Until recently, most studies on the surgical clipping and endovascular treatment of brain aneurysms were either small-scale or retrospective studies that relied on analyzing historical case records. The only multi-centre prospective randomized clinical trial – considered the gold-standard in study design – comparing surgical clipping and endovascular coiling of ruptured aneurysm is the International Subarachnoid Aneurysm Trial (ISAT).
The study found that in patients equally suited for both treatment options, endovascular coiling treatment produces substantially better patient outcomes than surgery in terms of survival free of disability at one year. The relative risk of death or significant disability within one year of being treated with coils was 22.6 percent lower than in surgically-treated patients.
The study results were so compelling that the trial was halted early after enrolling 2,143 of the planned 2,500 patients because the trial steering committee determined it was no longer ethical to randomize patients to neurosurgical clipping. Long-term follow-up will be essential to assess the durability of the substantial early advantage of endovascular coiling over conventional neurosurgical clipping for the treatment of brain aneurysms.
It is important to note that patients enrolled in the ISAT were evaluated by both a neurosurgeon and an endovascular coiling specialist, and both physicians had to agree that the aneurysm was treatable by either technique. However, this study provides compelling evidence that, if medically possible, all patients with ruptured brain aneurysms should receive an endovascular consultation as part of the protocol for the treatment of brain aneurysms.
Although no multi-centre randomized clinical trial comparing endovascular coiling and surgical treatment of unruptured aneurysms has yet been conducted, retrospective analyses have found that endovascular coiling is associated with less risk of bad outcomes, shorter hospital stays and shorter recovery times compared with surgery.
(The author is Associate Consultant Neuroradiology at Sri Balaji Medical Institute, New Delhi)