Back pain STILL remains a mystery

Back pain is the most common cause of disability in most countries across the globe. 8 out of 10 people will suffer from a significant episode during their lifetime…….
By Dr Harvinder Singh Chhabra
We should all be aware about the red flags which indicate that immediate opinion should be taken from a clinician for needful. If along with back pain one has malaise, that is a general feeling of discomfort, weakness, or lack of well-being, or fever, night sweats, loss of appetite, or weight loss, it is one such red flag.
If not treated, timely and properly spinal infections can result in serious consequences like paralysis and spinal deformity and even a significant potential for mortality with rates ranging up to 4%.
Spinal infections can be bacterial, viral, or fungal. The most common cause is bacterial which could be pyogenic or tubercular. Tubercular Spine is quite common in India and other emerging countries and contributes significantly to the burden of non-traumatic spinal cord injuries and spinal deformity.
Non-specific clinical presentation makes spinal infections a major diagnostic and treatment dilemma. There is often a significant delay between first symptoms and diagnosis leading to devastating consequences in some cases.

Low back pain still remains a mystery for most people. It often starts without any warning and without any obvious reason, interferes with daily activities and a comfortable night’s sleep, and then just as unexpectedly the pain subsides.
When in acute pain we desperately seek relief from the pain. But as soon as we recover from an acute episode, we tend to forget about the problem. Once we develop recurrent low back pain, we have to seek assistance time and again, to become pain free.
80 – 85% of people will suffer from a significant low back pain at some point of their life time, In US it is the second most common ailment after common cold. What compounds this bad news is the fact that nearly 70% of sufferers will have a recurrence within one year of the initial episode.
The seriousness of chronic low back pain is often emphasized in terms of the hair-raising economic costs of work absenteeism ( it is responsible for the highest number of man hours lost in the industry , but it may well be far worse than that — a recent Swedish study shows that it probably even shortens lives.
However, the good news is that most episodes of back pain will last only a short time (upto 75% recover in three months), only 1-3% of back problems would require surgery and a healthy lifestyle helps.
Mechanical back pain is among the most common causes of back pain where the pain aggravates with activity and is relieved by rest. Sedentary lifestyles and improper postures are two main reasons why back pain has assumed epidemic proportions. Amongst the other predisposing factors are professions requiring manual work / prolonged improper posture / sedentary work, obesity, stressful life style, pregnancy and previous history of back pain.
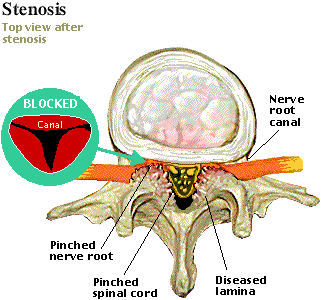
A number of structural problems may also result in back and leg pain which include bulging/ ruptured discs, arthritis, spinal canal stenosis (narrowing of the spinal canal),scoliosis(abnormal curvature of the spine), spondylolisthesis (one vertebra slipping forward over another vertebra), infection, osteoporosis (brittle and porous bones), tumours and referred pain(pain from other areas of the body like kidney/ureter/uterus may radiate to the back and cause back pain).
Investigations like MRI are advised if the back pain fails to resolve with conservative trial of more than 6 weeks, if back pain occurs after an injury or fall or if back pain is associated with difficulty in bladder/ bowel control, weakness in legs, fever or with unexplained weight loss.
Diffusion tensor imaging (DTI) and tractography, MR spectroscopy (MRS),Positron emission tomography (PET), Single photon emission computed tomography (SPECT), Functional MRI (fMRI) of the spinal cord are some of the latest advancements in diagnosis of spine disorders

The management of back pain could be divided into two parts – general treatment which is common for any kind of ailment of the back and treatment specific to the ailment causing back pain. The general treatment could further be divided into two parts – treatment of the back pain and reducing the chances of recurrence of back pain.
The role of conservative management cannot be underrated in spine disorders. Removal of predisposing factors, maintaining proper postures, aerobic general conditioning exercises and specific back exercises are the main stay of conservative management along with medications. The Updated Cochrane Review of Bed Rest for Low Back Pain and Sciatica suggested that for people with acute low back pain, advice to rest in bed is less effective than advice to stay active. For patients with sciatica, there is little or no difference between advice to rest in bed and advice to stay active.
Unnecessary surgery should be avoided. Conversely, when conservative management has failed surgery should not be unduly delayed Back pain is generally treated by heat (hot fomentation / short wave diathermy / ultrasonic therapy etc.) / ice packs, massage and drugs. Generally ice packs are more effective during an acute episode of back pain (first 48 hours) whereas heat is more effective after the acute phase. However, this may not hold true for everyone and one needs to find by trial and error as to what gives maximum relief. Massage should be gentle and no sudden jerk or torsional strain should be applied. Non steroidal anti-inflammatory drugs should be used only for a limited period.
Prolonged use of these drugs can cause serious side effects on the gastrointestinal system, kidney and heart. In fact there are more deaths in the US due to the side effects of these drugs than due to AIDS. However this does not mean that these drugs are not to be used at all and are just “pain killers”. They reduce the inflammation and thus relieve the pain thereby helping the individual to be up and around earlier. If there is an associated pain travelling down the leg (like in sciatica), the doctor may prescribe additional drugs like Pregabalin.


The second part of the treatment, i.e. reducing the chance of recurrence is equally, if not more important. For this one has to try to remove the predisposing factors. Adequate amount of general conditioning exercises like walks, treadmill, aerobics, swimming etc need to be incorporated into one’s normal lifestyle. 4 kms of walks at a stretch or its equivalent of another general conditioning exercise up to 4 days in a week is sufficient. In addition, the muscles of back could also be strengthened by stretching / yogic exercises.
To maintain a normal posture, one should maintain the normal curves in the spine at all times, whether in sitting, lying or working position. One should use a proper chair when sitting for a long time, mattress on the bed should not sag, one should not slouch in the bed or chair and should not be in one position for long hours (one could change the posture every 40-50 minutes while sitting). Modifying the workplace environment may be very important.
Trying to maintain one’s weight, conditioning the back muscles after pregnancy and taking suitable steps to tackle the mental stress are other important aspects to reduce the chance of recurrence.
If a herniated (prolapsed inter vertebral) disc does not respond to general treatment one may need to go in for epidural injections or surgery. Transforaminal epidural steroid injections under fluoroscopic guidance are safe and up to 60 percent of patients who do not respond to a comprehensive conservative treatment, get long term relief with three such injections thus obviating a surgery. Spine surgery has seen advancements in operative techniques, implants and biologics, and equipment such as computer-assisted navigation and surgical robotics increasing the safety and accuracy of surgery.
Intraoperative neuro-monitoring has increased the bar of safety in spine surgery, particularly in cases with kyphosis, scoliosis, or pre-existing neurological impairment. Any potential insult to the cord can be detected immediately so that remedial measures can be taken immediately.
 Spine surgery could be done by traditional open or minimally invasive techniques. Minimally invasive spine surgery techniques reduce the need for larger incisions and reduce muscle dissection. They carry less blood loss and postoperative pain; reduce the length of hospital stay and patients return to normal activities sooner. Thus in surgery for prolapse intervertebral disc, the budging disc could be removed by traditional, microscopic or endoscopic procedures. In Endoscopic disectomy a tubular retractor is placed by dilation of muscles rather than splitting of muscles in traditional technique. A light source and camera is placed on the tubular retractor thus enabling a magnified image of surgical field with good illumination. The surgery is carried out through this tubular retractor.
Spine surgery could be done by traditional open or minimally invasive techniques. Minimally invasive spine surgery techniques reduce the need for larger incisions and reduce muscle dissection. They carry less blood loss and postoperative pain; reduce the length of hospital stay and patients return to normal activities sooner. Thus in surgery for prolapse intervertebral disc, the budging disc could be removed by traditional, microscopic or endoscopic procedures. In Endoscopic disectomy a tubular retractor is placed by dilation of muscles rather than splitting of muscles in traditional technique. A light source and camera is placed on the tubular retractor thus enabling a magnified image of surgical field with good illumination. The surgery is carried out through this tubular retractor.
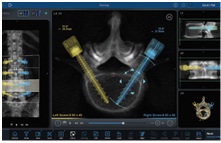
Spine surgery relies upon meticulous fine motor skills to manipulate neural elements and a steady hand while doing so, often exploiting small working corridors. These procedures may also be long and arduous, predisposing the surgeon to both mental and physical fatigue. Spinal robotics and navigation are the latest development in spine surgery and are making life easier for the surgeon. They represent promising potential for improving modern spinal surgery. These platforms may mitigate much of the harmful radiation exposure in minimally invasive surgery to which the patient, surgeon, and ancillary operating room staff are subjected.
The fluoroscopy time gets reduced. They also increase the accuracy of screw placement and facilitate larger screw insertion, stronger fixation and significantly fewer revision procedures. Robotic spine surgery, for example, has increased accuracy to 98-99%, reduced radiation exposure (74% as compared to C-arm and 50% as compared to navigation), reduced complication rate and reduced the length of hospital stay18. The main drawback in these procedures is the cost involved.
Mobility and stability are equal partners in the structure of the human spine as determined by our need, function, and purpose of action: to survive and excel. Hence, various innovative motion preserving surgeries have been developed to obviate the adverse effects of the traditional fusion surgery. Nowadays a disc replacement surgery can be done. When the disc needs to be removed, rather than going for a fusion surgery which by placing additional stress on the adjoining segments, predisposes to adjacent segment degeneration and increased rates of re-surgery, the disc could be replaced, thus preserving motion. Posterior dynamic stabilization(mobile screw parts, mobile connectors or a combination of both), interspinous spacers, facet joint replacement and nucleus replacement are other latest motion preserving techniques. However, a balance between the extent of mobility of the implant to avoid an overload of the bone–implant interface and an effective stabilization of the spinal motion segment must be found.
Vertebroplasty and kyphoplasty are minimally invasive surgical techniques to treat vertebral compression fractures due to osteoporosis or trauma where bone cement is injected into the vertebra, the cement hardens, stiffens the fracture and supports the spine.
Spinal cord stimulation (SCS) is a proven safe and effective therapy that can help to manage many types of chronic intractable pain. It uses low voltage (electrical) stimulation of the spinal nerves to help block the sensation of pain. To achieve SCS, a small battery-powered generator is implanted under the skin to transmit an electrical current to the spinal cord. The electrical current generated interrupts pain signals being sent to the brain and an individual being treated generally feels pain relief. It is important to understand that stimulation does not eliminate the source of pain; it simply interferes with the signal to the brain.
Thanks to smart phones and mobile apps, our lives have become much easier. Mobile health is emerging as the most convenient way to deliver services remotely, and collect outcomes in real time, thus contributing to disease management by transferring care from hospital to home. It also facilitates back pain management through not only providing accessibility to healthcare, but also enhancing patients’ understanding of their condition, and their willingness to engage in self-management so vital for back pain management, giving way to high-quality care to the satisfaction of both patients and healthcare professionals. Nowadays, there are mobile apps like Snapcare which are meant to help people with back pain and to teach them self-care of the back.
 With advances in understanding the cell biology and characteristics of the intervertebral disc at the molecular and cellular level that have been made, alternative strategies for addressing disc pathology can be discovered. Areas of promise currently that are being actively investigated include mesenchymal stem cell infusion, cell isolation and reconditioning, platelet rich plasma(PRP) infusion, and tissue engineering and biomaterial-based strategies.
With advances in understanding the cell biology and characteristics of the intervertebral disc at the molecular and cellular level that have been made, alternative strategies for addressing disc pathology can be discovered. Areas of promise currently that are being actively investigated include mesenchymal stem cell infusion, cell isolation and reconditioning, platelet rich plasma(PRP) infusion, and tissue engineering and biomaterial-based strategies.
To summarise, back ailments and pain has afflicted mankind since a long time, but has assumed epidemic proportions in the last two decades. We have come a long way ahead in the field of spine. Spine care, like all of medicine, is challenging. Spine surgery has become safer and simpler with the new techniques and advancements. However, the indications and inherent limitations of the latest techniques have to be borne in mind.
A wise surgeon could help you understand the various treatment options available for your problem, explaining the risks and benefits of each of them. Do not hesitate to take a second opinion. Get a wise advice and save yourself from the agony of chronic low back pain.
(The author is Medical Director, Department of Spine care Sri Balaji Action hospital New Delhi)

