Elevating Liver Health
 Liver health is a critical yet often overlooked aspect of overall well-being. It is imperative to know the intricate functions of this organ and effectively combat the rising prevalence of liver diseases. Double Helical explores the challenges, innovations, and expert insights shaping the prevention, diagnosis, and treatment of liver ailments.
Liver health is a critical yet often overlooked aspect of overall well-being. It is imperative to know the intricate functions of this organ and effectively combat the rising prevalence of liver diseases. Double Helical explores the challenges, innovations, and expert insights shaping the prevention, diagnosis, and treatment of liver ailments.
By abhigyan / Abhinav
Liver, an indispensable organ, executes over 500 essential tasks crucial for maintaining bodily functions. Its pivotal role in digestion includes detoxification, protein synthesis, and the production of digestive enzymes vital for breaking down food. As a cornerstone of the digestive system, the liver’s health is paramount.
Historically, civilisations recognised the liver’s significance dating back to ancient times. In 2000 BC, the Babylonians esteemed the liver, understanding its centrality in bodily functions, long before the discovery of the heart. Analogously, the liver is often likened to a pillar supporting the body, emphasising its structural robustness and importance. Despite its resilience, negligence towards liver health can lead to severe consequences. While the liver initially tolerates dietary and lifestyle indiscretions, prolonged neglect can result in adverse outcomes.
Positioned in the right upper abdomen beneath the rib cage, the liver’s anatomical and functional complexity is remarkable. Categorically, the liver serves two major functions: excretory and synthetic. It metabolises most foreign substances and waste products before excreting them via bile or the kidneys. Proper bilirubin excretion is critical, as defects in this process can lead to jaundice.
Furthermore, the liver is the primary site for synthesising major proteins crucial for various bodily functions. Bile synthesised in the liver aids in fat digestion, while the organ also plays a pivotal role in fat and carbohydrate metabolism, underscoring its metabolic significance.
Symptoms of Liver Disease
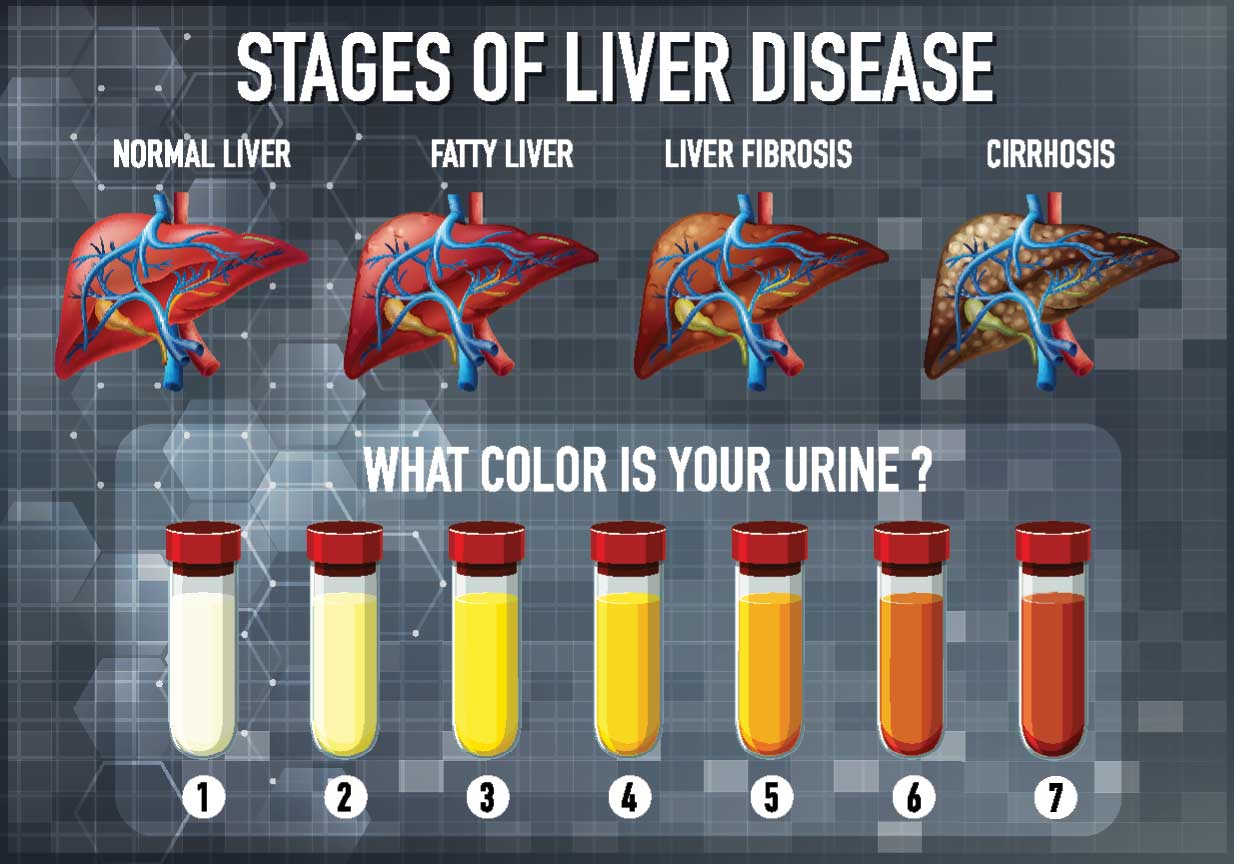
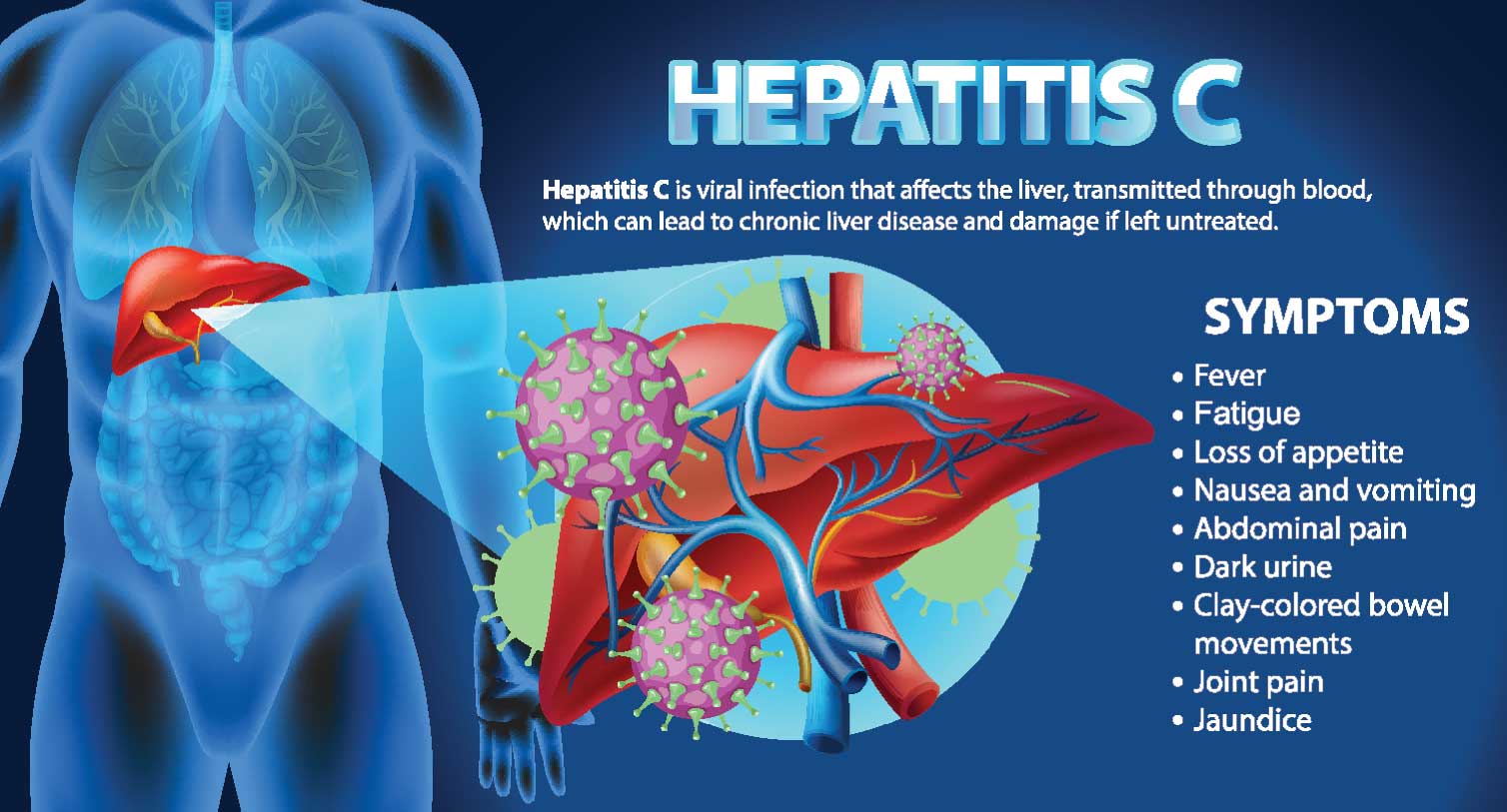
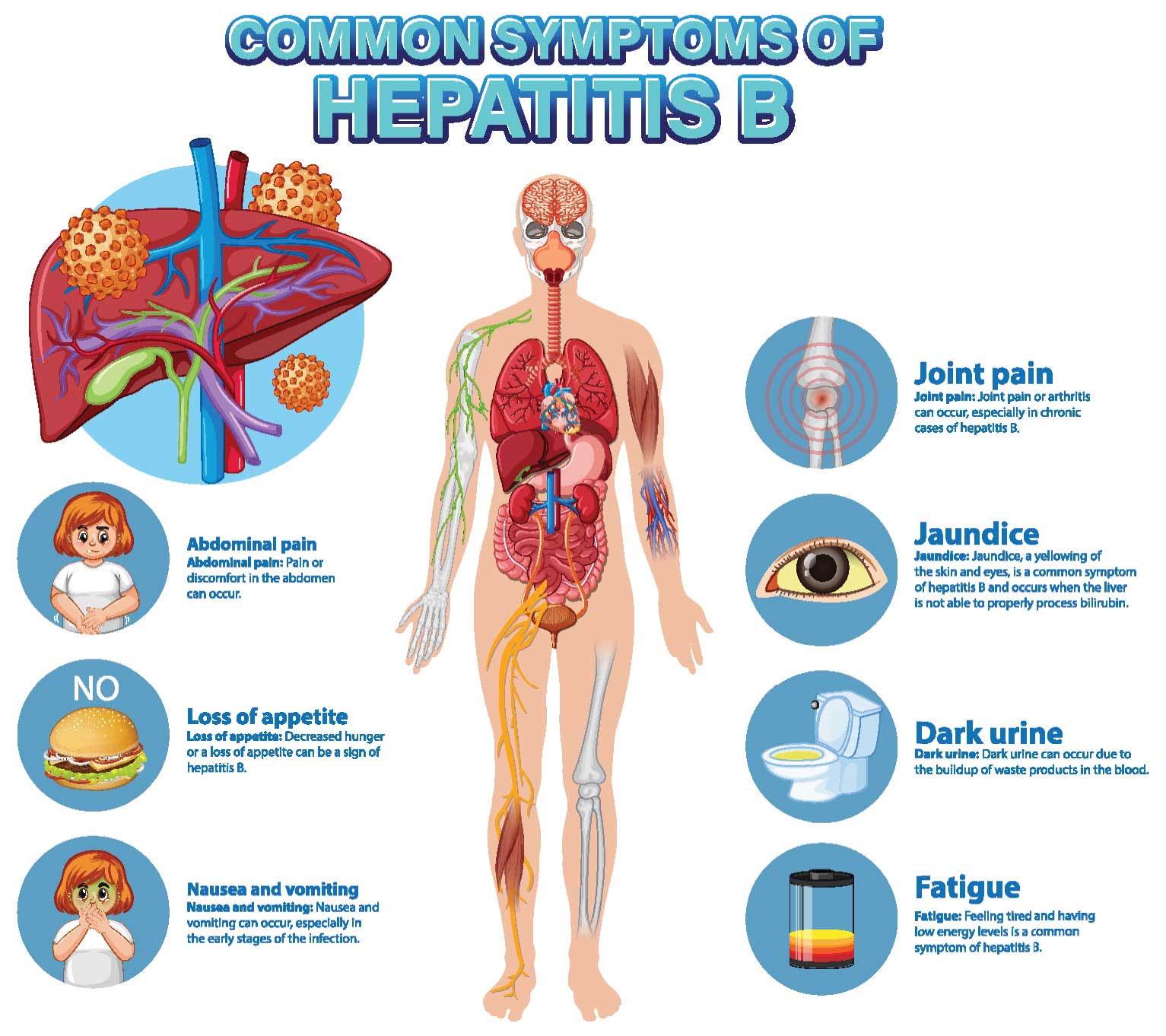
Liver diseases often present with non-specific symptoms in their early or mild stages, such as fatigue or weakness. However, significant liver injury can manifest as jaundice, characterised by the yellow discoloration of the sclera of the eyeball and dark yellow urine. Liver cirrhosis, resulting from persistent damage due to causes like alcohol consumption or hepatitis B and C infections, presents with symptoms such as ascites, loss of consciousness (coma), and gastrointestinal bleeding.
Types of Liver Disease
Liver diseases encompass short-lasting, self-limiting conditions, and smouldering slow diseases, which can cause permanent damage like liver cirrhosis. Among hepatitis viruses, Hepatitis A and E typically lead to jaundice, resolving without causing long-term liver damage. However, Hepatitis B and C infections can lead to chronic liver diseases and cirrhosis, posing significant challenges globally. Preventive measures such as vaccination against Hepatitis A and B and public awareness campaigns are vital in controlling these infections.
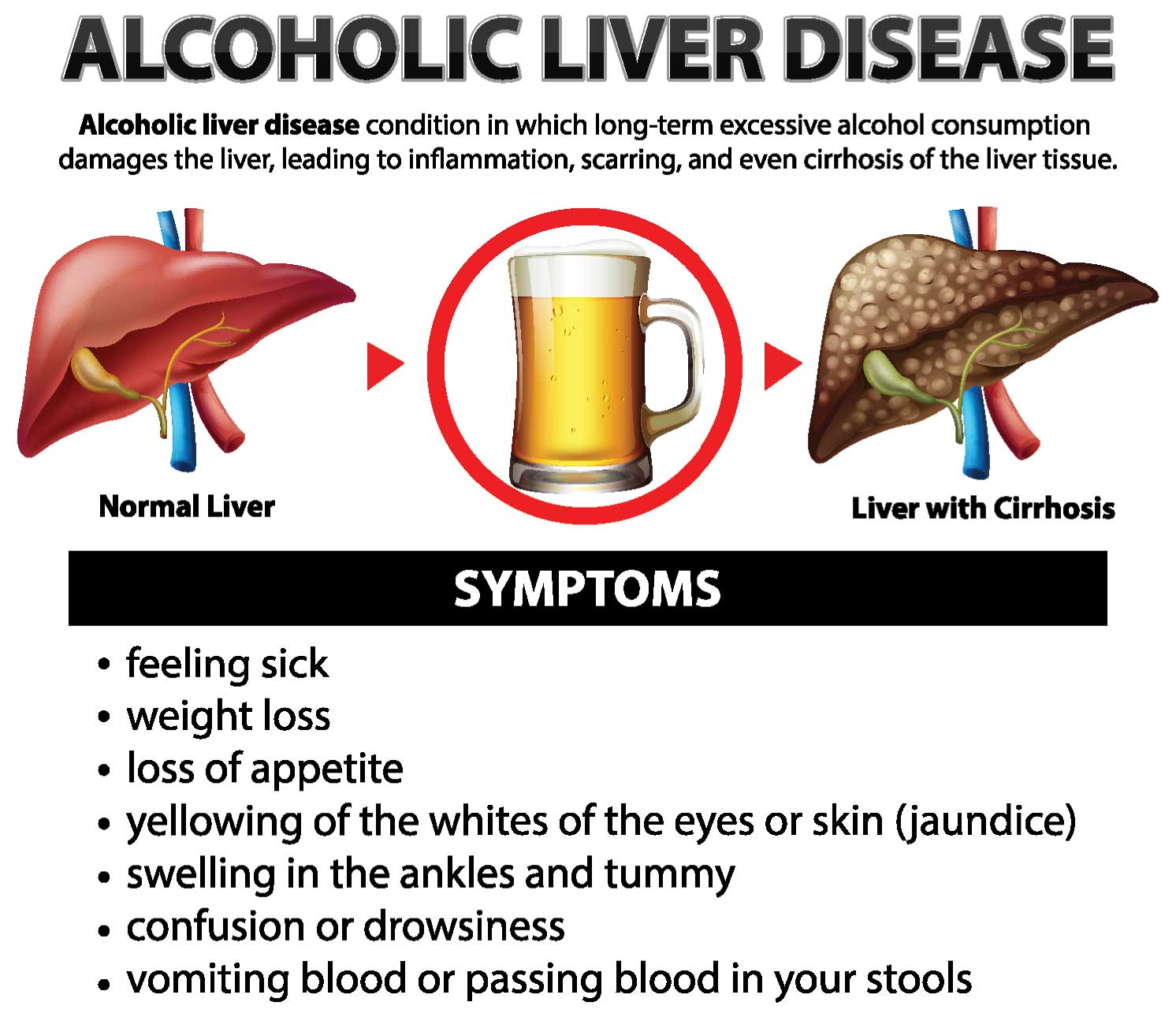
Alcohol Consumption and Liver Disease
Alcohol consumption remains a significant cause of liver diseases, with over 48 percent of liver disease cases at ILBS attributed to high alcohol intake. Despite its social acceptance, alcohol abuse has led to increased consumption across all social, age, and gender groups. Raising awareness about responsible alcohol consumption and destigmatising seeking help for alcohol-related issues are imperative in preventing liver diseases associated with alcohol abuse.
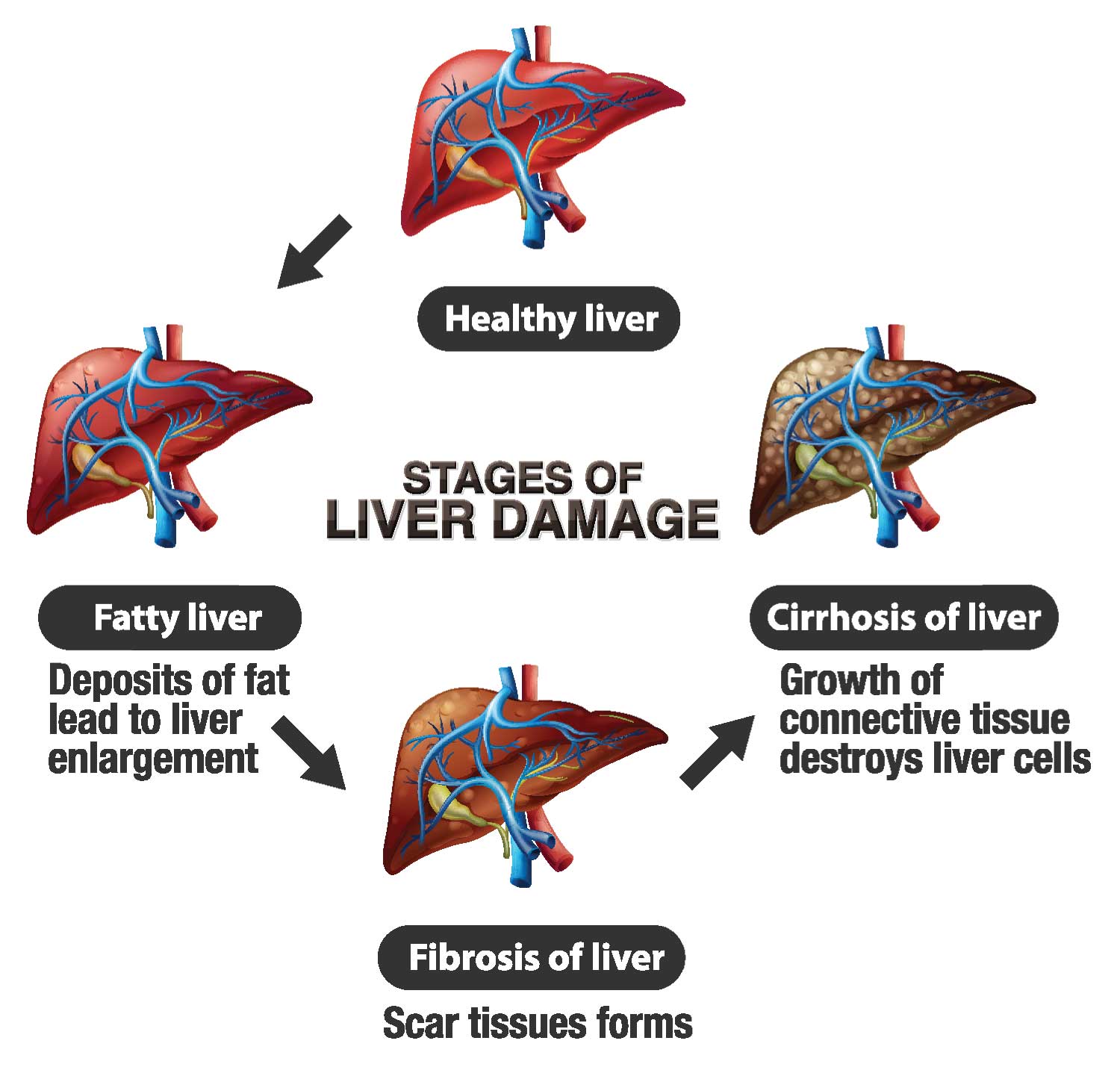
Fatty liver disease, characterised by the accumulation of excess fat in the liver, is a prevalent condition often detected incidentally during routine ultrasound examinations or liver function tests. While it progresses slowly, in a substantial number of cases, it can lead to liver cirrhosis over years to decades. The primary causes of fatty liver disease are attributed to obesity and diabetes, with the global epidemic of these lifestyle diseases contributing to its rise. In fact, in the Western world, fatty liver disease has become the second most common cause of liver cirrhosis, following hepatitis C. Prevention remains pivotal in managing fatty liver disease, with lifestyle modifications such as adopting a healthy diet being more effective than medication in its early stages.
Fatty liver disease serves as a precursor to various systemic problems. Excessive calorie intake leads to fat build-up in the liver, impairing its normal processing and breakdown functions, resulting in fat accumulation. Individuals with obesity, diabetes, or high triglycerides are prone to developing fatty liver disease. Although fatty liver may initially cause no damage, excess fat can lead to liver inflammation. Elevated glucose levels, characteristic of pre-diabetes or overt diabetes, further contribute to triglyceride synthesis, exacerbating hepatic fat accumulation.

While many individuals with fatty liver disease remain asymptomatic, it can progress to liver damage in some cases. Fortunately, lifestyle changes can often prevent or even reverse fatty liver disease. It is important to note that up to 72 percent of individuals with underlying liver disease exhibit no symptoms. Common symptoms, when present, are non-specific and include fatigue, lack of drive, and itching. Factors such as obesity and alcohol consumption have emerged as key risk factors for liver disease, alongside historically prevalent viral hepatitis. However, advancements in prevention strategies and treatment have led to improving trends in chronic liver disease outcomes.
Treatment and Prevention Strategies
Several measures can aid in the treatment and prevention of liver disease:
Avoidance of Cigarettes and Alcohol: Given their detrimental effects, avoiding cigarettes and excessive alcohol consumption is crucial in preventing liver disease.
Hepatitis B Vaccination: Vaccination against hepatitis B is essential in preventing chronic liver infections and cirrhosis.
Needle Safety: Avoiding the reuse or sharing of needles helps prevent blood borne infections, including hepatitis B and C.
Promoting Voluntary Blood Donation: Enhancing surveillance of blood products and promoting voluntary blood donation can reduce the risk of transfusion-related liver infections.
Obesity Management: Controlling obesity through healthy lifestyle choices, including regular exercise and a balanced diet, is vital.
Safe Drinking Water: Ensuring access to safe drinking water helps prevent waterborne liver infections.
Medication Safety: Avoiding the non-judicious use of drugs and sticking to prescribed medications is essential.
Healthy Dietary Habits: Opting for homemade food over outside food and adopting a balanced diet in fruits, vegetables, and whole grains supports liver health.
 Leading the Way in Liver Care
Leading the Way in Liver Care
Dr S K Sarin, as Chancellor and Director of the Institute of Liver and Biliary Sciences (ILBS), has made remarkable contributions to liver research and clinical practice. Renowned as a gastroenterologist and hepatologist, he has pioneered clinical innovations and made significant strides in medical education. Dr Sarin’s protocols for the primary prevention of variceal bleeding and management of gastric varices have become standard practices globally. His extensive work on hepatitis and cirrhosis management, including liver regeneration using growth factors, has provided hope for patients with advanced liver disease. Moreover, his efforts in preventing mother-to-baby transmission of hepatitis B have been instrumental in protecting newborns from chronic HBV infection. Dr Sarin’s tireless dedication to liver health continues to positively impact countless lives worldwide.
ILBS stands as a beacon of excellence, offering cost-effective and comprehensive liver care services in the region. Dr Sarin, renowned as a gastroenterologist and hepatologist, has made indelible contributions to medical education, clinical innovations, and research.
 His groundbreaking work in liver disease management has revolutionised the field. Dr Sarin’s protocols for the primary prevention of variceal bleeding and management of gastric varices have become global standards. Additionally, his research on liver regeneration using growth factors offers hope for patients with advanced liver disease, providing options for transplant-free survival.
His groundbreaking work in liver disease management has revolutionised the field. Dr Sarin’s protocols for the primary prevention of variceal bleeding and management of gastric varices have become global standards. Additionally, his research on liver regeneration using growth factors offers hope for patients with advanced liver disease, providing options for transplant-free survival.
Dr Sarin’s dedication extends beyond clinical practice. He has led the development of numerous treatment guidelines, including spearheading major Asian Pacific treatment protocols in liver diseases.
ILBS, under Dr Sarin’s leadership, continues to serve as a centre of excellence, offering cutting-edge treatments, comprehensive care, and groundbreaking research in liver and biliary sciences. Dr Sarin’s tireless commitment to liver health underscores his status as a pioneer in the field, shaping the future of liver care worldwide.
Dr S K Sarin has made remarkable contributions to liver research and clinical practice. Renowned as a gastroenterologist and hepatologist, he has pioneered clinical innovations and made significant strides in medical education. Dr Sarin’s protocols for the primary prevention of variceal bleeding and management of gastric varices have become standard practices globally.
Dr S K Sarin’s contributions to liver research and clinical innovations have significantly impacted the field. His work on variceal bleeding management and hepatitis treatment protocols has set global standards. Additionally, his efforts in liver regeneration and preventing mother-to-baby transmission of Hepatitis B showcase his dedication to improving liver health worldwide. As Chancellor and Director of the ILBS, Dr Sarin continues to spearhead advancements in liver care, offering comprehensive solutions and hope for patients with liver diseases.