Rising Tide of Diabetes
 The epidemiology of diabetes in India presents a unique scenario influenced by both “nature” and “nurture” factors, set against a backdrop of malnutrition across the life course…
The epidemiology of diabetes in India presents a unique scenario influenced by both “nature” and “nurture” factors, set against a backdrop of malnutrition across the life course…
By Dr Amitav Banerjee
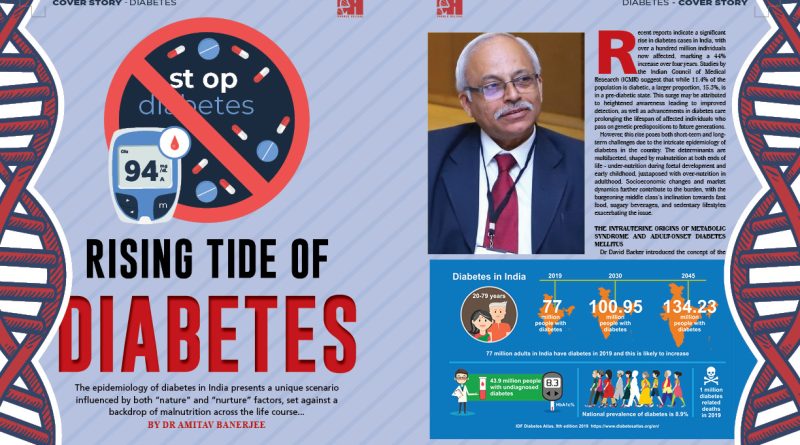
Recent reports indicate a significant rise in diabetes cases in India, with over a hundred million individuals now affected, marking a 44% increase over four years. Studies by the Indian Council of Medical Research (ICMR) suggest that while 11.4% of the population is diabetic, a larger proportion, 15.3%, is in a pre-diabetic state. This surge may be attributed to heightened awareness leading to improved detection, as well as advancements in diabetes care prolonging the lifespan of affected individuals who pass on genetic predispositions to future generations.
However, this rise poses both short-term and long-term challenges due to the intricate epidemiology of diabetes in the country. The determinants are multifaceted, shaped by malnutrition at both ends of life – under-nutrition during foetal development and early childhood, juxtaposed with over-nutrition in adulthood. Socioeconomic changes and market dynamics further contribute to the burden, with the burgeoning middle class’s inclination towards fast food, sugary beverages, and sedentary lifestyles exacerbating the issue.
The Intrauterine Origins of Metabolic Syndrome and Adult-Onset Diabetes Mellitus
Dr David Barker introduced the concept of the foetal origins of adult disease (FOAD), popularly known as the Barker’s hypothesis. This theory posits that events during early developmental stages, particularly intrauterine conditions, significantly influence the risk of developing diseases in adulthood. Low birth weight, indicative of intrauterine growth restriction, predisposes individuals to insulin resistance, obesity, and cardiovascular diseases later in life.
Barker’s hypothesis underscores the impact of inadequate nutrition during foetal development, programming the foetus with metabolic characteristics that increase susceptibility to future diseases. Individuals undernourished in utero are more prone to obesity and its associated conditions, including type 2 diabetes, during adulthood.

The Thrifty Gene Hypothesis
The thrifty gene hypothesis endeavours to elucidate the elevated prevalence of obesity, metabolic syndrome, diabetes mellitus, and cardiovascular diseases in populations undergoing rapid economic growth. It posits that genetic traits conducive to fat accumulation around the waist, known as central obesity, conferred survival advantages during periods of scarcity such as famines. Populations that have endured such famine experiences are believed to harbour a higher proportion of individuals with the “thrifty gene,” as per Darwinian principles, adapting to endure harsh conditions compared to those lacking this genetic predisposition. India, with its history of severe famines like those in Agra, Bihar in the nineteenth century, and the Bengal famine in the twentieth century under British rule, likely hosts a significant proportion of individuals with this genetic profile.
However, this adaptive “genetic programming,” beneficial during times of famine, becomes detrimental in times of caloric abundance. Populations previously subjected to deprivation, now experiencing rapid economic growth and expanding middle class, often indulge in excess fast food consumption while reducing physical activity. The persistence of thrifty genes from past eras of famine and deprivation contributes to the high prevalence of metabolic syndrome—a combination of central obesity, increased insulin resistance, diabetes mellitus, and vascular and neurological complications like coronary events and stroke.
While the thrifty gene hypothesis offers a coherent explanation for the lay audience, evidence supporting this theory remains a work in progress.
Life Course Strategy to Change Destiny
As depicted in the superhit movie “Muqaddar Ka Sikandar,” where “Muqaddar” symbolises destiny and “Sikandar” represents a conqueror, a significant portion of Indians carry a genetic predisposition due to past adversities like famines or early-life under-nutrition, putting them at risk for developing metabolic syndrome. This can be considered their destiny or handicap. To overcome this, a life course approach is essential to mitigate the burden of diabetes and metabolic syndrome in the long term.
The latest National Family Health Survey (NFHS-5), 2019-21, unveiled alarming statistics: 36% of under-five children in India are stunted, 19% are wasted, and 32% are underweight, all indicators of early childhood malnutrition. These children, predominantly born to mothers with low educational attainment and in the lowest wealth quintile, may have experienced intrauterine growth retardation. Furthermore, nearly 20% of newborns in India have low birth weight, indicating intrauterine growth restriction.

These children, facing foetal and early childhood nutritional deficiencies, are at heightened risk of developing diabetes and metabolic syndrome in adulthood. To prevent future generations of under-nourished children from contributing to the cycle of adult diabetes, urgent interventions are needed to address maternal and child under-nutrition.
What about those unable to escape the fate of early-life malnutrition? They too can alter their destiny by resisting lifestyles that predispose them to risks—the “nurture” aspect. While genetic predispositions or early-life deprivations may elevate the risk of metabolic syndrome in a large portion of individuals in low-income countries, lifestyle choices can play a pivotal role in managing metabolic syndrome and its related conditions. Behaviour and environment can influence gene expression, optimising health outcomes and preventing the manifestation of adverse genetic traits.
Diet and Exercise: Overcoming Genetic Handicap
Genetic predispositions are not immutable; with the right lifestyle modifications, individuals can achieve optimal health despite these inherent challenges. Many early diabetics and pre-diabetics can attain optimal health through lifestyle changes, including adopting a healthy diet, engaging in regular physical activity, abstaining from sugar, tobacco, and alcohol, and maintaining an ideal body weight. Some diabetics may even reduce or eliminate their anti-diabetic medications through disciplined adherence to this lifestyle. However, any adjustments to medication should be made under the expert supervision of a physician.
Given the widespread risk within our population, a population-wide approach to prevention is crucial. Promoting better maternal and early childhood nutrition, along with advocating for physical activity and healthy diets across the life course, will have a lasting impact on diabetes control within the population.


Obstacles to Lifestyle and Population Approach
Market forces and misleading role models present significant barriers to the adoption of healthy lifestyles at both individual and population levels. The strong influence of market forces targeting the newly affluent population poses a major challenge. Furthermore, the endorsement of sugary soft drinks and colas by popular sports figures, who serve as role models, is distressingly common. However, there are notable exceptions, such as Pullela Gopichand, the Indian badminton star, who refused to endorse a soft drink brand at the height of his career.
Secondary Prevention: Care for Diabetics
In managing diabetes, primary care should play a pivotal role, especially considering the limited number of endocrinologists available. Primary care providers are the linchpins of diabetes management in the community. However, this role is increasingly challenging due to the growing complexity of anti-diabetic medications, the need for meticulous monitoring of blood sugar levels, and the imperative to prevent both hypo- and hyperglycaemia, alongside providing counselling on lifestyle modifications.
Patient’s Role in Diabetes Management
In chronic conditions like diabetes, the patient’s role in management is crucial, if not paramount. Self-monitoring of blood glucose levels using a glucose meter and HbA1c testing, which measures average blood sugar levels over three months, are common methods for monitoring diabetes. Patients can easily learn self-glucose monitoring techniques.
Recent advancements in diabetes management include continuous glucose monitoring (CGM) technology, which offers the potential to enhance overall glycaemia control while minimising hypoglycaemia. However, widespread adoption of CGM technology is still limited.
Patients should also receive education on foot care, as diabetic foot complications are common. Smoking cessation, moderation or abstinence from alcohol consumption, regular eye screenings for cataracts and retinopathy, kidney function tests, and cardiac function tests are essential for identifying any involvement of target organs.
Exercise, adherence to a balanced diet, and proper use of anti-diabetic medications under the supervision and periodic review of a physician are crucial measures for managing this chronic condition.
(The author is a Professor at DY Patil Medical College, Pune, and an Academic Editor at PLOS ONE.)