Insights on Cerebral Intruders
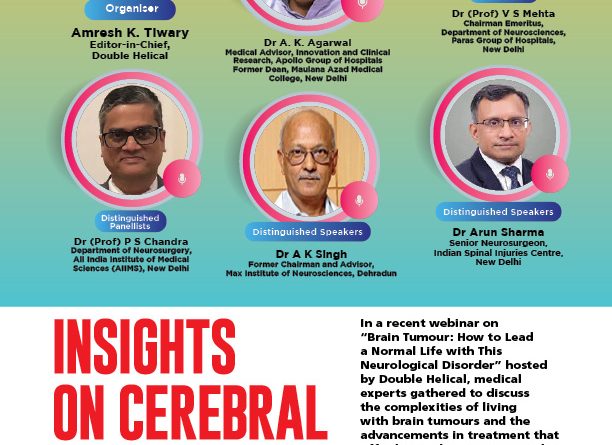
In a recent webinar on “Brain Tumour: How to Lead a Normal Life with This Neurological Disorder” hosted by Double Helical, medical experts gathered to discuss the complexities of living with brain tumours and the advancements in treatment that offer hope. The session aimed to demystify the fear surrounding neurological disorders, shedding light on the importance of early detection, effective treatments, and the resilience of those affected by brain bumps.
The webinar featured a distinguished panel of speakers, including renowned experts and leading specialists in the medical field. Among them were Dr V S Mehta (Chairman Emeritus, Department of Neurosciences, Paras Group of Hospitals, New Delhi), Dr P S Chandra (Department of Neurosurgery, All India Institute of Medical Sciences, AIIMS, New Delhi), Dr A K Singh (Former Chairman and Advisor, Max Institute of Neurosciences, Dehradun), and Dr Arun Sharma (Senior Neurosurgeon, Indian Spinal Injuries Centre, New Delhi).
Dr A K Agarwal, Professor of Excellence and Former Dean of Maulana Azad Medical College, as well as Medical Advisor for Clinical Research and Innovation at Apollo Group Hospital, New Delhi, moderated the session, while Amresh K Tiwary, Editor-in-Chief, Double Helical welcomed the participants and articulated the viewer’s queries. Excerpts…
Dr A K Agarwal: A very good morning to all my colleagues, esteemed panellists, and the entire audience joining us through YouTube. Double Helical, a magazine dedicated to health awareness, has, over the last ten years, provided invaluable information to the public and the medical profession, benefiting countless individuals. Amresh K Tiwary, the key person behind Double Helical, has chosen a critical topic this time: how to navigate the fear surrounding brain tumours. The moment individuals learn they have a tumour, especially a brain tumour, the immediate reaction is often fear and anxiety about what lies ahead. Our discussion today will centre on detection, treatment, and rehabilitation.
Let’s begin by addressing a common misconception: the word “tumour” often evokes fear, particularly when it pertains to the brain. This raises an important question: in what ways is a brain tumour different from other types of tumours, and why does it evoke such fear?
Dr A K Singh: Good morning, everyone. This is a very pertinent question, but it encompasses multiple layers. First, it’s important to understand that the term “brain tumour” includes both cancerous and non-cancerous tumours, each with different prognoses. The brain controls every function of the body—movement, speech, understanding, and vision—so when the brain is affected, it can impair the functioning of these body parts. The brain acts as the CPU of the body, and any problems here can lead to significant challenges in quality of life, even if one manages to survive. Additionally, our minds tend to linger on negative outcomes, often focusing on stories of individuals who have faced dire consequences, rather than recognising the many who have survived and thrived.

Dr Agarwal: As you mentioned, the brain’s role in controlling the body means that any tumour can lead to various symptoms, depending on its location. Dr Mehta, given your extensive experience as a neurosurgeon, how do you perceive the trends in brain tumour cases? Are we seeing an increase, and if so, is it due to heightened awareness and improved diagnostic facilities?
Dr V S Mehta: You’re absolutely right. We are observing an increase in the detection of brain tumours, primarily due to advancements in imaging technologies such as MRI and CT scans, which are now widely accessible. Increased public awareness has also played a significant role; people no longer dismiss mild headaches or visual disturbances as minor issues. Instead, they seek diagnostic imaging at the first signs of symptoms, leading to earlier detection of tumours.
Dr Agarwal: So, technological advancements and public awareness are crucial in early detection. What symptoms should the public be vigilant about? Unlike breast cancer, where self-examination is possible, how can individuals monitor for potential brain tumours?
Dr Mehta: As Dr A K Singh pointed out, different areas of the brain govern different functions. Symptoms can vary widely depending on the tumour’s location. For instance, a tumour in the frontal lobe may lead to cognitive impairment, while one in the motor area could result in weakness. The most common symptom associated with brain tumours is headache, particularly when persistent, progressive, and accompanied by other symptoms such as visual loss or vomiting. Individuals experiencing these symptoms should seek an MRI or CT scan. Furthermore, tumours originating from the pituitary gland can disrupt hormonal balance, causing conditions like galactorrhea and amenorrhea in women or loss of libido in men. Tumours affecting cranial nerves can also produce symptoms, such as hearing loss or seizures, especially in adults, which should prompt immediate investigation for potential brain tumours.
Dr Agarwal: I think you have covered some of the common symptoms for which the public should be aware. It’s worth noting that increasing headache is perhaps the initial symptom, along with seizures, and obviously, the symptomatology will vary depending on the location of the tumours, as you have already described. Dr Mehta, based on your experience, what do you think is the ratio of benign to malignant tumours out of 100?
Dr Mehta: I would estimate that about one-third, or 30 per cent, of brain tumours are malignant, while nearly 70 per cent are benign. Benign tumours usually produce symptoms due to pressure on specific nerves, whereas malignant tumours tend to invade or arise from brain tissue. The symptoms of benign tumours typically occur due to pressure on particular areas of the brain, while cancerous tumours involve more extensive brain tissue. Once deficits appear from a benign tumour, you can expect improvement following its removal, as the symptoms are primarily due to pressure. However, if patients present at later stages, irreversible damage may occur, and improvement might not be possible. In contrast, with cancerous tumours, our aim is to halt further progression by removing the tumour, extending the patient’s life, and then considering radiation and chemotherapy.
Dr Agarwal: Proceeding to Dr Chandra, as Dr Mehta mentioned, there’s a 30-40 per cent possibility of malignant tumours, with the majority being benign. Based on your experience, what are the most common benign brain tumours, and what are their typical symptoms? I know this question has been touched upon, but could you elaborate on the common benign tumours and their individual symptomatology?
Dr P S Chandra: That’s a very good question. I would like to reiterate that approximately 10 per cent of patients come in with incidental benign brain tumours. We are seeing this more frequently due to increased access to imaging, as Professor Mehta mentioned. Nowadays, anyone with a headache often requests imaging, and the threshold for doing so is very low. Many patients insist on getting an MRI to rule out any serious conditions, leading to the discovery of benign tumours, which then prompts them to seek surgical opinions. The most common incidental tumour is meningioma, which is most often found in women. The most common presentation is some form of non-specific headache, which leads to imaging.
In my practice, I can recall at least 20 to 30 patients who simply come for follow-up MRIs over two or three years and remain asymptomatic; we do nothing else for them. Additionally, the most common benign tumours include meningiomas, which can occur anywhere in the skull. Other types of pathologies include cavernomas, which are not exactly tumours but have a tendency to bleed.
The location of these tumours is also crucial, as it impacts the outcome significantly. For instance, a pituitary adenoma is a completely benign tumour, but its location at the base of the skull means it can affect the visual pathways, leading to vision loss. This makes complete removal challenging, and patients may present with visual disturbances and hormonal imbalances.
Similarly, tumours located in eloquent areas of the brain, such as the motor cortex, can present with weakness in the hands and legs. The surgical removal of these tumours can be tricky because complete removal could lead to neurological deficits. Nowadays, we have advanced techniques that allow us to perform surgeries under awake monitoring, enabling us to map the motor cortex effectively.
Another set of benign tumours can present with seizures, such as gangliogliomas, which are common in women aged 20 to 30 and are often found in the temporal lobes. Patients typically present solely with seizures, and these tumours may not grow. In such cases, we operate primarily to control their seizures or epilepsy. There are also benign tumours called dysembryonic neuroepithelial tumours (DNETs), which remain stable in size throughout a patient’s life, necessitating surgical intervention.
It’s essential to consider the following factors when assessing benign tumours: a) Whether the patient has presented with symptoms or if the tumour was discovered incidentally through scanning, leading to unnecessary panic. b) The tumour’s location—whether it’s in a non-eloquent or eloquent area. c) The extent to which the tumour can be confidently removed. For instance, lower-grade gliomas must be completely excised; otherwise, there is a risk of malignancy or recurrence.
To summarise, the term “brain tumour” encompasses a wide variety of conditions, and the public often perceives it as a single entity. When they see someone severely affected, they panic and worry about their own health. Hence, it’s crucial for individuals to seek expert opinions to understand the specific category of their brain tumour, its implications, necessary surgical interventions, and expected outcomes.
Dr Agarwal: Thank you, Dr Chandra. I’ll now switch over to Dr Arun Sharma. Welcome to this seminar, Dr Arun Sharma, a leading neurosurgeon from Indian Spinal Injury, New Delhi—a place that has made a significant name in the field of neurosciences and related areas. Dr Arun, I would like to ask, as Dr Chandra has nicely described, which malignant brain tumours do you find to be the worst variety, and what is their symptomatology? I often refer to them as “bombs within our brain.”
Dr Arun Sharma: The most common malignant tumours are usually glioblastomas, which tend to occur more frequently in the elderly, but recently we’ve been observing them in individuals in their 40s and 50s as well. They grow rapidly, and patients typically present with either chronic headaches lasting a short duration, like 2 or 3 months, or with symptoms such as speech difficulties or limb weakness. These are among the most common presentations for glioblastomas.
Dr Agarwal: Indeed. What can you tell us about the progression of this particularly dangerous brain tumour? How does it manifest from the day it’s detected compared to seven days later? How can the patient realize that it is something growing very quickly, and what observations do you, as a clinician, make?
Dr Sharma: Glioblastomas are very aggressive. By the time a patient learns about their condition, the prognosis is typically poor. The median survival with a good quality of life is usually between 6 to 18 months. However, there are instances where individuals survive longer due to radiation therapy, chemotherapy, and effective surgical excision. Overall, the prognosis remains unfavourable, and families are often left devastated and depressed upon receiving this diagnosis. After surgery, patients generally undergo radiotherapy and chemotherapy. Unfortunately, recurrence is common, typically occurring within six months to two or three years. Many patients experience recurrence within the first 18 months, with some developing tumours larger than the original, despite the best efforts at treatment.
Dr Agarwal: Thank you, Arun. Now, let me turn back to Dr AK Singh. I find it intriguing to reflect on your early experiences in neurosurgery. When you began your career, you would diagnose brain tumours, correct? How did the diagnostic methods in the 1970s compare to today’s practices?
Dr A K Singh: Indeed, our diagnostic capabilities were very limited back then. We primarily relied on some modalities. The first was an angiogram, where we would insert a needle into the neck’s carotid artery to examine the blood vessels for abnormalities. The second involved injecting a contrast agent into the brain’s cavities (the ventricles) to assess distortions, which helped us estimate the location of lesions based on clinical presentations. This required significant effort and an in-depth knowledge of anatomy. Nowadays, with advancements in CT and MRI, we have access to 3D imaging of any pathology within the skull, making it easier to visualise the size and location of tumours. This advancement has simplified our job considerably and has reduced the neurological deficits that might arise from surgery.
Dr Agarwal: Clearly, over the past 50 years, the ease of diagnosis has improved significantly. Prompt detection and surgical intervention, as opposed to relying solely on other treatment protocols, have shown better outcomes. What can you say about the satisfaction of patients from your early years to now?
Dr Mehta: In those early days, it was mentally and physically challenging. Operations would begin at 8 AM and often conclude around 10 PM, without breaks for food. It required immense physical stamina. Afterward, we would spend the night monitoring patients to ensure they didn’t encounter major complications. Today, the process is much more manageable. Most surgeries now take only three to four hours. Diagnostic tools and surgical techniques have improved significantly. In the 70s, we relied on monopolar cautery, and we lacked access to microscopes or endoscopes. We also didn’t have mechanical ventilation, which are all standard today. The advancements in anaesthesia and coagulation techniques have dramatically improved our ability to differentiate between normal and abnormal tissue, leading to safer outcomes for patients.
Dr Agarwal: It sounds like the landscape has changed profoundly. Earlier, brain tumour surgeries had a mortality rate of 50 per cent to 70 per cent, making it a dire prognosis. What’s the current situation regarding mortality rates?
Dr Mehta: Now, the mortality rate around surgery is reduced to approximately 1 per cent, often even less. Patients are recovering much more rapidly post-surgery. If a patient presented with only a headache or seizures, they could often be eating, drinking, and talking within 24 hours after the operation. The difference is indeed remarkable.
Dr A K Agarwal: Thank you. The key message is that while having a brain tumour is undoubtedly serious, advancements in detection and treatment over the past few decades have dramatically improved outcomes. As you mentioned, early detection is crucial. I believe that two major advancements of the last century are imaging technology, particularly CT and MRI, and the development of endoscopic techniques.
Dr Singh: I completely agree!
Dr A K Agarwal: These innovations have transformed our ability to diagnose and treat neurological conditions, benefiting both patients and clinicians. Dr Mehta, how has your experience shaped your approach to dealing with brain tumours compared to the past?
Dr Mehta: In the last century, particularly over the last 50 years, the advancements in neuroscience have surpassed those in any other branch of medicine. As Dr A K Singh rightly pointed out, we used to rely on indirect methods, such as angiograms, to diagnose tumours. Without direct evidence of a tumour, we would infer its presence based on structural shifts, often leading to large craniotomies. This resulted in only partial resections, and we had little certainty about whether we had completely removed the tumour. Consequently, the prognosis was poor, with high rates of disability; operating on a brain tumour often meant the patient would suffer from hemiplegia or, in some cases, might not survive.
Today, the scenario has changed dramatically. We no longer accept that patients should develop new neurological deficits post-surgery; in fact, it is now rare for this to occur. Instead, we expect improvements in neurological function, depending on the tumour’s nature. For instance, a benign tumour pressing on brain structures may allow for recovery, while malignant tumours may leave some deficits that may or may not improve. Advances in technology, including image guidance, MRIs, perfusion MRIs, and functional MRIs, enable us to detail the tumour’s characteristics and its impact on patient function. With functional MRI, we can identify the hand area’s proximity to the tumour, allowing us to predict potential deficits. Surgeons now utilise image-guided surgery and electrophysiological monitoring to pinpoint motor areas accurately, allowing us to intervene during surgery if deficits arise.
Mortality rates in elective neurosurgery were notably high in the past. In 1997, I presented a paper advocating for zero mortality in this field. Today, we are proud to report that mortality rates are below one per cent, even prior to surgery.
Dr Agarwal: Thank you for providing hope to the people. The advancements in treatment mean that, although brain tumours are serious, the mortality rate of less than one per cent is a beacon of hope for patients and society alike.
Dr Chandra, having heard the discussions on the evolution of brain treatment, you are an experienced neurosurgeon, albeit somewhat younger than Dr A K Singh and Dr Mehta. Can you share the technologies that have facilitated your surgical practice and where you see the future heading?
Dr Chandra: That’s a pertinent question. I would categorise technologies into those that have caused a silent revolution and those responsible for an overt revolution. The overt revolution, as mentioned by Professors Mehta and A K Singh, includes remarkable advancements in imaging and intraoperative techniques.
The silent revolution encompasses significant developments in imaging. For example, we now routinely perform tractography to map brain tracts, allowing us to understand their localisation and functions during surgery. Additionally, intraoperative monitoring has seen a silent yet substantial evolution. While it has been in practice for a couple of decades, its adoption is now nearly universal in surgical centres. Techniques such as motor evoked potentials have become standard.
Surgeons today have refined their techniques significantly, with many adopting retractor-less neurosurgery, which minimises brain tissue retraction. This silent revolution is part of surgical training, enabling us to conduct surgeries without applying retraction on healthy brain tissue. Furthermore, intraoperative fluorescence techniques allow us to identify tumours during surgery.
Recent advances have also been made in the field of epilepsy surgery. We can now implant electrodes within the brain to map the networks causing epilepsy and remove both the tumour and the abnormal networks surrounding it safely.
These technologies are continuously evolving and being integrated into surgical practice, empowering surgeons with greater confidence. Neuronavigation, once considered a luxury, is now essential in most departments. Modern neuronavigation systems allow precise tumour localisation and include advanced algorithms to examine brain tracts and other critical areas.
As Professor Mehta noted, no other field has experienced such rapid advancement as neuroscience. It captivates interest, even drawing attention from figures like Elon Musk, who seek to understand the intricacies of brain function. This fascination drives technological evolution in the field.
Dr Agarwal: Thank you. This brings me to Dr Arun Sharma. Dr Chandra highlighted the advancements in neuronavigation, which the people are increasingly aware of. They may be curious about the availability of robotic surgical tools for brain tumours. Are they genuinely beneficial? Ultimately, our shared goal is precision in every step. What is your perspective on robotic surgery?
Dr Arun: While robotic surgery may not be prevalent in the field of neurosurgery, neuron navigation systems function similarly to robotics. Neuronavigation and intraoperative imaging significantly enhance our ability to define tumour boundaries, facilitating maximal tumour removal while ensuring good surgical margins with minimal retraction, as Dr Chandra has highlighted. Additionally, intraoperative MRI has been established in some centres, enabling us to assess the tumour’s status post-surgery. Thus, neuronavigation is comparable to robotic surgery in terms of its impact on surgical outcomes.
Dr Mehta: I’d like to add that robotic applications are an exciting frontier in neurosurgery. We have been using robotic systems for over seven years and have performed more than 600 cases. It’s important to note that there are various categories of robotic systems. The most complex category features robots that can plan and execute surgeries independently; however, this technology does not exist yet. Even the renowned da Vinci robotic systems ultimately rely on the surgeon’s control, as they lack true artificial intelligence.
In neurosurgery, current robotic devices primarily assist in achieving precise targeting, providing stability during procedures. For instance, they are instrumental in placing electrodes accurately in the brain for stereo electroencephalography, a technique vital for mapping abnormal neural networks in epilepsy. We have successfully placed over a thousand electrodes using this technology. Additionally, robots can assist in holding endoscopes for precise endoscopic surgeries and are increasingly used in minimally invasive procedures.
One notable application is in the treatment of complex epilepsies, such as laughing epilepsy, where a tumour located centrally in the brain causes uncontrollable laughter. Using robotic systems, we have developed electrodes to reach this challenging area and sever the connections between the tumour and the rest of the brain. We have published more than ten papers on these advancements. Recently, we have also employed robotic systems for a procedure called robotic-guided hemispheric disconnection, where we disconnect one half of the brain from the other to alleviate severe epilepsy in children experiencing hundreds of seizures daily. This technique has been documented in leading medical journals, demonstrating its effectiveness as a bloodless approach.
While the role of robotics in neurosurgery is currently limited, its potential is vast, and we eagerly anticipate further integration with artificial intelligence to enhance surgical capabilities.
Dr Agarwal: Thank you, Dr Chandra. It’s crucial to recognise the combination of robotics and AI, especially regarding brain tumours. However, I would like to revisit Dr A K Singh to discuss the importance of radiation and medical oncological support in treatment. There has been significant progress in medical oncology, particularly for malignant tumours. What is your perspective on this, considering the potential for improving patients’ quality of life?
Dr Singh: In terms of therapeutic options, we have radiation therapy, medical therapy, and immunotherapy. Radiation therapy plays a pivotal role in managing various tumour types, including benign ones. We employ techniques such as external beam radiotherapy and brachytherapy, with external beam radiotherapy being more common. There are three major modalities: standard therapy, CyberKnife, and Gamma Knife, each offering precision tailored to the tumour’s location.
Medical oncology has a more limited application in brain tumours compared to other cancers. Some brain tumours, particularly functioning pituitary tumours, respond well to hormonal or drug therapies. For malignant tumours, chemotherapy remains the primary option, extending survival by about 10 per cent when combined with radiation. Certain types, such as medulloblastomas, may also benefit from chemotherapy. Immunotherapy has been explored for approximately 30 years, but results have been mixed, and no widely effective treatment has emerged for the most common and devastating brain tumour, glioblastoma multiforme.
Dr Agarwal: Thank you, Dr Singh, for that overview of treatment modalities. Dr Mehta, there is a lot of buzz around high-frequency MRI-guided ultrasound therapy in medical journals and on social media. Can you shed some light on its status?
Dr Mehta: I’ve seen those reports as well. However, I must emphasise that my knowledge in this area is limited, and currently, it remains largely experimental. While ultrasound-guided therapies have shown promise in non-brain tumour cases, such as urological tumours, the evidence for treating brain tumours specifically is still lacking. Focused ultrasound has been used successfully to create lesions for seizure management, but its efficacy in tumour treatment is not yet well established.
Dr Agarwal: It’s essential to convey that as these therapies are still in experimental stages, we must approach them with caution, especially for patients seeking immediate solutions.
Dr Singh: Indeed. The interest in alternative therapies often stems from a lack of perfect solutions. While ultrasound has been effective in creating lesions for conditions like seizures, its application for tumours is still under research, with no long-term data supporting its efficacy in that context.
Dr Mehta: We are set to install focused ultrasound technology at AIIMS within six months, which will expand our treatment options. Currently, there is only one facility in India providing this treatment at a high cost. Our goal is to offer it more affordably. As Professor A K Singh mentioned, the FDA has approved focused ultrasound primarily for treating Parkinson’s disease-related tremors. While some studies indicate potential for epilepsy treatment, the indications are still being defined.
Dr Agarwal: In conclusion, patients suffering from brain tumours deserve access to the best possible treatment modalities to enhance their quality of life. Given that India has a vast population, we should strive to provide these advanced treatments to our citizens, bridging the gap compared to the Western world. Let us work together to improve the quality of life for our patients.
Amresh K Tiwary: One viewer asks if you could share success stories of patients with brain tumours who have resumed fulfilling lives post-treatment.
Dr Chandra: Certainly! Many patients with benign tumours lead normal lives after treatment. Initially, there may be postoperative deficits, but most patients improve over time. If they experience seizures, we often continue antiepileptic medications for a period, but we can stop these once they are seizure-free for several years and if follow-up MRI confirms no tumour presence.
(With Inputs from Janhvi Verma)