Battling a Latent Peril
India faces significant challenges in achieving its ambitious goal of eliminating tuberculosis by 2025. The high prevalence of latent TB infection (LTBI) within its population, poverty, malnutrition, indoor air pollution from cooking stoves, urban overcrowding, delayed diagnosis, inconsistent treatment, and various other contributing factors complicate efforts to combat this pervasive disease.
By Dr N K Prasanna & S K Varshney


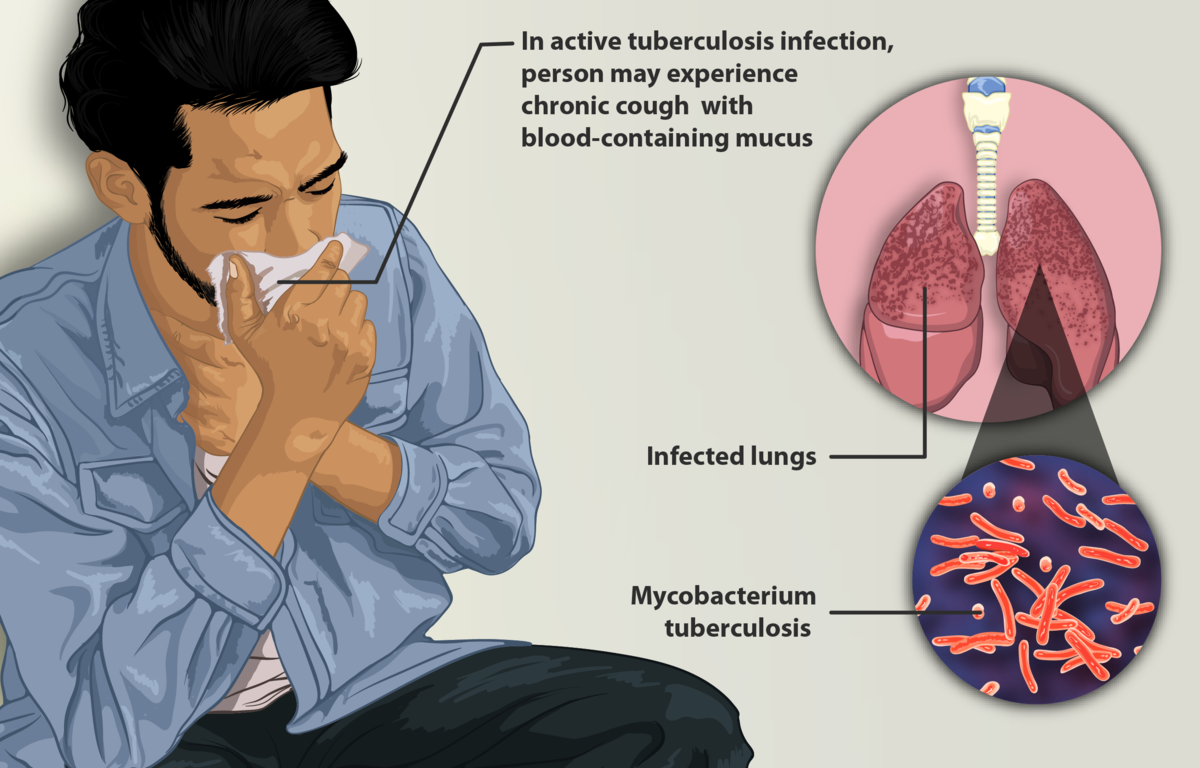
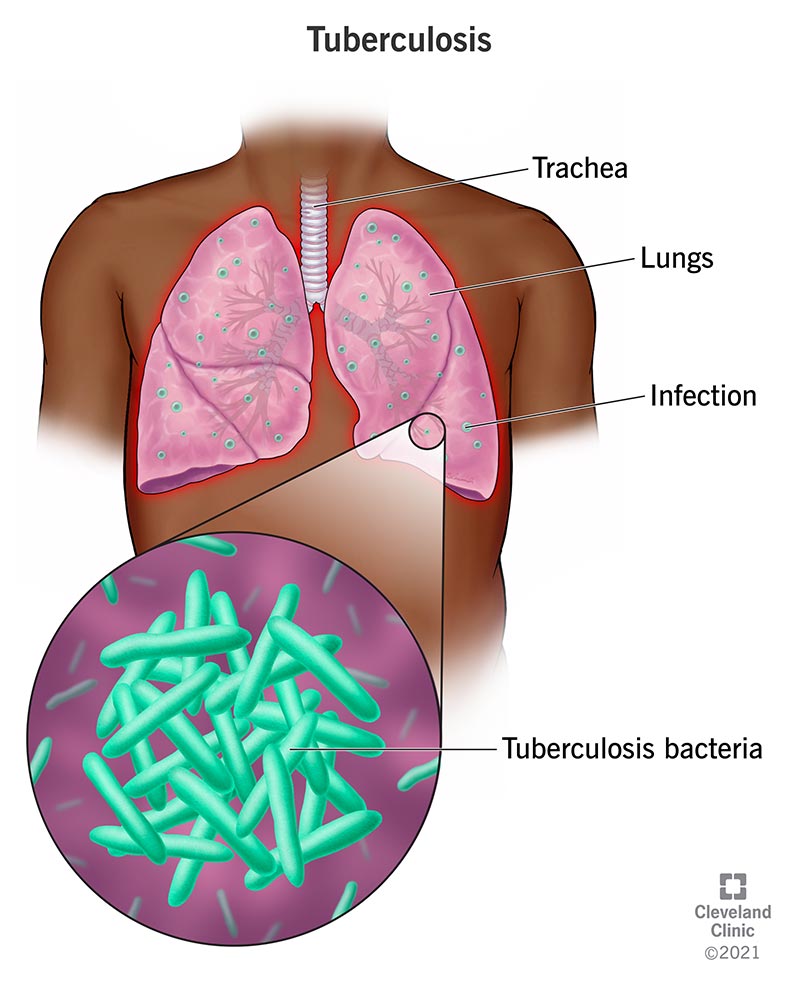
Tuberculosis, or TB, is a serious infectious disease caused by the bacterium Mycobacterium tuberculosis. While it mainly targets the lungs (a condition known as pulmonary TB), it can spread to other parts of the body, causing extra-pulmonary TB, which affects areas such as lymph nodes, the pleura (the protective membrane surrounding the lungs), bones, joints, the genito-urinary tract (including kidneys, bladder, and testes), the abdomen (including intestines, peritoneum, and mesentery), and even the skin.
In pulmonary TB, typical symptoms include a persistent cough lasting more than two weeks, a prolonged fever, noticeable weight loss, night sweats, coughing up blood, chest pain, weakness, and fatigue. In cases of extra-pulmonary TB, the symptoms vary depending on which body part is affected. For example:
• Swelling in lymph nodes,
• Joint pain and swelling,
• Stiffness in the neck or mental disorientation, and
• General symptoms such as significant weight loss, continuous fever for over two weeks, and night sweats.
India’s National TB Programmes
The Indian government initiated a National Tuberculosis Programme (NTP) in 1962, specifically to control TB. In 1997, this evolved into the Revised National TB Control Programme (RNTCP), which aimed to scale up TB control measures nationwide. By 2005, the entire country was covered under this programme. For the next decade, India aimed to meet the Millennium Development Goals (MDGs) and the global Stop TB Partnership targets for controlling the disease. In 2017, the Government of India (GOI) set an ambitious target to eliminate TB by 2025, aligning this goal with the Sustainable Development Goals (SDGs) to accelerate efforts and create an impact. To support this goal, in 2019, the RNTCP was renamed the National Tuberculosis Elimination Programme (NTEP). The National Strategic Plan (NSP-2017) envisions a TB-free India with zero TB deaths, zero disease, and no poverty due to TB.

Impact of COVID-19 on TB Control
The COVID-19 pandemic presented unprecedented challenges in TB control efforts. Although TB notifications temporarily declined during India’s major COVID-19 waves, the NTEP reported a 19% increase in TB cases in 2021 compared to 2020. This makes the goal of a TB-free India by 2025 more challenging, as gaps remain in providing free diagnostic services and medication. Effective TB management still hinges on early detection, correct treatment, and breaking the chain of transmission. Furthermore, extensive awareness programs for both rural and urban populations across India are crucial to inform people about TB, its prevention, and treatment.
The global impact of TB remains staggering. In 2020 alone, around 1.5 million people died from the disease. According to the World Health Organization (WHO), India bears 27% of the global TB cases and an alarming 35% of TB-related deaths, highlighting the urgent need for intervention. India has set ambitious elimination targets, and the Indian Council of Medical Research (ICMR) is exploring innovative approaches to tackle this public health crisis.
How TB Spreads
Contrary to historical beliefs that TB was genetically transmitted, it is now known that TB spreads through the air. In 1882, Robert Koch identified Mycobacterium tuberculosis (often called the tubercle bacillus), revealing its airborne transmission. TB bacteria are spread via tiny droplets released when a person with lung TB (particularly if TB bacteria are present in their sputum) coughs, sneezes, or even talks. These droplets remain airborne and can be inhaled by others, reaching deep into the lungs. Covering the mouth when coughing or sneezing—using a handkerchief, cloth, hand, or elbow—helps reduce transmission.

The progression from TB infection to active disease is influenced by several factors. Those at a higher risk include individuals with other lung diseases, those undergoing immunosuppressive treatment, smokers, and those with diabetes. The body’s response to TB bacteria begins with an influx of immune cells, including polymorphonucleocytes (PMNs) and macrophages, at the infection site. Over time, macrophages take over, forming a lesion called a tubercle (or Ghon’s focus) in the lung, which may eventually calcify.
Challenges in TB Elimination in India
India faces significant hurdles in eliminating TB, stemming from widespread latent TB infection (LTBI) within its population. This latent infection can become active at any time, especially in individuals with weakened immunity. Many Indians suffer from undernutrition and health conditions, such as diabetes, that make TB reactivation more likely. Furthermore, environmental factors like indoor air pollution from cooking stoves or smoking exacerbate the risk of active TB.
Urban overcrowding accelerates TB transmission across all socioeconomic levels, further complicating containment efforts. Although TB control has proven possible globally with adequate diagnosis and treatment, delayed diagnosis and inconsistent treatment are persistent issues in India. Many patients, particularly those in the private healthcare sector, struggle with the prolonged and expensive treatment process. While the public sector offers a better success rate, one-third of patients are still lost between seeking care and achieving a full cure.
Moreover, India has a significant burden of multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB cases, with most cases remaining undetected and untreated. Even when detected, treatment is prolonged, costly, and often leads to poor outcomes.
To eradicate TB, it is essential to address underlying issues, such as poverty, malnutrition, diabetes, and substance use. Poverty and TB are interlinked, with underprivileged children being particularly vulnerable due to weakened immunity, poor living conditions, and lack of access to healthcare. Crowded and poorly ventilated homes create an ideal environment for TB bacteria to spread. Successfully reducing TB requires a comprehensive approach that includes poverty alleviation, equal access to healthcare, better living conditions, and improved educational opportunities for underprivileged communities.
DOTS: The Backbone of TB Treatment
Directly Observed Treatment, Short-course (DOTS) is an effective TB treatment strategy that involves healthcare workers or family members observing patients as they take their medication. This ensures adherence to the treatment regimen, which is vital to preventing drug resistance and achieving successful outcomes. Most TB patients in India live below the poverty line, with some earning less than Rs 2000 per month. DOTS has proven successful in managing TB among economically disadvantaged populations, emphasising the importance of targeted support to enable timely diagnosis and treatment.
A clear understanding of TB, its transmission, and symptoms is crucial to early detection and treatment. Implementing DOTS and supporting vulnerable populations through financial assistance and healthcare access are key steps to reducing TB’s burden. India’s 2025 TB elimination target is ambitious, and achieving it requires continued efforts in awareness, prevention, diagnosis, and sustainable treatment solutions.
MoHFW-Revised National Tuberculosis Control Programme (RNTCP)
The Revised National Tuberculosis Control Programme (RNTCP) Launched in 1997, the RNTCP is grounded in the internationally recognised Directly Observed Treatment Short-course (DOTS) strategy, which emphasises the importance of directly observed treatment to ensure adherence and minimise the risk of drug resistance. By integrating these evidence-based practices, the RNTCP aims to effectively reduce the morbidity and mortality associated with TB in the country.
One of the key features of the RNTCP is its commitment to providing free diagnosis and treatment services to all TB patients, thereby addressing the economic barriers that often prevent individuals from seeking care. The program facilitates access to high-quality diagnostic tests, such as sputum smear microscopy and chest X-rays, as well as providing essential anti-TB medications at no cost. This comprehensive approach not only promotes early detection and timely treatment but also encourages individuals from vulnerable populations to seek help without the fear of financial burden.
TB: Global health challenge (MDR-TB):
Multi-drug-resistant tuberculosis (MDR-TB) is a grave concern in the field of public health. It refers to a strain of tuberculosis that has developed resistance to the two most potent first-line drugs used for its treatment – isoniazid and rifampicin. This resistance makes MDR-TB significantly more challenging to treat and control. The greatest challenge faced in TB control today is reaching the unreached populations. Despite significant progress made in TB prevention and treatment, there are still millions of people who lack access to proper healthcare services, especially in low-income countries with limited resources. This creates a breeding ground for MDR-TB, as inadequate or incomplete treatment can lead to the development of drug resistance.
Another factor is a lack of awareness and education about TB and its prevention among these vulnerable populations. The stigma associated with the disease further hinders efforts to control its spread, as individuals may be reluctant to seek diagnosis and treatment. To effectively address this challenge, it is crucial for governments, international organisations, and healthcare providers to prioritise reaching these unreached populations with comprehensive TB control programs. This includes improving access to diagnostics, ensuring the availability of quality-assured drugs, strengthening healthcare infrastructure in underserved areas, and implementing robust strategies in community engagement. Without addressing these issues efforts towards controlling MDR-TB will remain incomplete, posing a significant threat not only to individual health but also to global public health security.
Impact of education on TB awareness and its social and medical implications: Education plays a crucial role in raising awareness about tuberculosis and its multifaceted implications for individuals and communities. By informing people about the causes, symptoms, transmission, and prevention of TB, educational programs can significantly reduce stigma associated with the disease. Misunderstandings surrounded by TB often lead to social isolation of affected individuals, exacerbating mental health issues and hindering their ability to seek timely medical care. Through targeted awareness initiatives, we can foster a supportive environment that encourages individuals to seek treatment without fear of discrimination.
Moreover, an educated populace is better equipped to understand the medical ramifications of TB, including its potential to develop into drug-resistant forms if left untreated. Public health education campaigns can empower individuals with knowledge about the importance of adhering to treatment regimens and the consequences of non-compliance. This understanding not only enhances individual health outcomes but also curtails the spread of TB within communities, thereby addressing broader public health concerns. Conversely, the lack of education about TB can result in delayed diagnoses and treatment, which can have dire social and medical consequences, amplifying the burden of the disease on health systems and society at large. By investing in educational resources and initiatives, societies can create a more informed citizenry that recognises the importance of prevention, early detection, and treatment of TB.
Indian Initiatives in elimination of TB: The ICMR RATIONS trial has shed light on an intriguing correlation between nutritional support and the reduction of TB incidence. This study highlights how providing adequate nutrition alongside standard treatment can potentially contribute to improved outcomes in TB patients. India has taken significant initiatives to combat tuberculosis through various programs and campaigns. One of the key initiatives is the Pradhan Mantri TB Mukt Bharat Abhiyan, which aims to make India TB-free by 2025 which leverage the activities of Corporate Social Responsibility (CSR). This program focuses on strengthening the healthcare system, improving access to quality diagnosis and treatment, and creating awareness about TB prevention.
The National Strategic Plan (NSP) for Tuberculosis Elimination (2017-2025) is an important initiative aimed at eradicating tuberculosis in the country. India has set ambitious targets to eliminate TB. The plan includes strategies such as early diagnosis, effective treatment regimens, and ensuring patient-centred care. To raise awareness among the general public, the government launched the “TBHarega, DeshJeetega” campaign. This campaign aims to educate people about TB symptoms, importance of early detection, and adherence to treatment. It also encourages individuals to come forward for testing if they experience any symptoms or have been in contact with TB patients.
Project GATIMAN
To realise the ambitious objective of a TB Mukt Bharat (TB-free India), WHO-India is launching Project GATIMAN, a comprehensive initiative designed to bolster technical assistance across critical areas such as public-private partnerships, TB surveillance, knowledge management, implementation research, drug-resistant TB management, laboratory capacities, and effective advocacy and communications at both state and union territory levels. This multifaceted approach aims not only to strengthen the infrastructure for tackling tuberculosis but also to ensure that essential resources and support are accessible where they are needed most. Recognising the challenges posed by difficult-to-reach and neglected regions, WHO-India has strategically identified and committed to supporting 100 such districts, demonstrating a focused effort to address the disparities in TB care and to ultimately eradicate the disease from the nation’s landscape. Through these concerted efforts, Project GATIMAN is set to make significant strides toward the vision of a TB-free India, empowering communities and revitalising health systems in the process.
Nikshay Poshan Yojana is an initiative launched by the Government of India aimed at enhancing the nutritional status of patients suffering from tuberculosis. Understanding that proper nutrition is crucial for the recovery and overall health of TB patients, this program provides a monthly financial incentive of Rs. 1000 to all notified TB patients. This support not only alleviates some of the financial burdens associated with the disease but also encourages patients to maintain a healthy diet, which is essential for their treatment and recovery. By ensuring that TB patients receive adequate nutrition, the Nikshay Poshan Yojana plays a vital role in improving treatment outcomes. Malnutrition can significantly affect the body’s ability to combat infections, and by addressing this issue, the scheme aims to enhance the immune response of patients. The direct cash transfer allows individuals and families to purchase nutrient-rich foods, thereby facilitating better adherence to treatment protocols. These comprehensive efforts by the Indian government demonstrate a strong commitment towards combating TB and achieving a healthier nation. Together, let us work towards creating a future where no individual suffers from this preventable and treatable disease – a future where every life counts.
CSIR’s Efforts in Tuberculosis Research
The Council of Scientific and Industrial Research (CSIR) is one of India’s premier research and development organisations, known for its contributions to health and medicine. The CSIR launched the ‘Open Source Drug Discovery’ (OSDD) initiative to create a global consortium aimed at developing affordable treatments for tuberculosis. This was initiated to ensure that new TB medications are accessible and affordable in India, which has the highest TB burden. So in collaboration with the TB Alliance, CSIR focused on fostering local drug development and also partnered with Cadila Pharma, to create ‘Risorine,’ a new drug formulation that enhances the effectiveness of Rifampicin without the need for high doses.
ICMR-National Institute of Research for Tuberculosis: NIRT, a prominent institute under the umbrella of Indian Council of Medical Research, focuses on advancing the fight against tuberculosis by enhancing diagnosis, treatment, and monitoring through research and clinical trials. It supports the DOTS strategy in India’s TB control program, emphasises high standards of patient care, and improves research integrity through peer review and competitive funding. It also integrates various scientific disciplines to understand TB and its impacts, which offers training for researchers, and promotes collaboration between public and private sectors, through knowledge dissemination to develop effective TB control strategies. It also upholds ethical research practices and protects intellectual property rights.
The research activities at NIRT are dedicated to the comprehensive study of bacteriology, immunology, epidemiology, socio-behavioural science, and clinical pharmacology, with a relentless focus on combating tuberculosis. Despite significant advances, the battle against this formidable disease is far from over, prompting ongoing investigations into the evolving principles of chemotherapy and related immunological factors. By maintaining rigorous scientific standards, NIRT ensures that its research efforts not only contribute valuable insight into tuberculosis but also enhance our understanding of the socio-behavioural aspects that influence its spread and treatment.
Impact of tuberculosis in low and middle income countries: A closer look
The India TB Report 2024 reveals a decline in tuberculosis mortality from 28 to 23 per lakh population between 2015 and 2022. Key findings include an increase in private sector case notifications, with 33 per cent of reported cases in 2023 coming from private sources, up from 1.9 lakh in 2015. The estimated TB incidence rose slightly to 27.8 lakh in 2023, maintaining a mortality rate of 3.2 lakh. India met its goal of initiating treatment in 95 per cent of diagnosed patients but faces challenges in eliminating TB by 2025 due to risk factors like undernourishment (7.44 lakh affected in 2022), HIV (94,000 TB patients), and diabetes (1.02 lakh diabetic TB patients). Screening for alcohol and tobacco use revealed that 7.1 per cent and 11 per cent of patients, respectively, were users.
TB remains a significant global health issue, with millions affected annually and a high mortality rate, particularly among those with HIV. The majority of individuals affected by tuberculosis (TB) reside in low- and middle-income countries. Even though, TB is found globally, half of the total TB cases are concentrated in eight countries: Bangladesh, China, India, Indonesia, Nigeria, Pakistan, the Philippines, and South Africa.
Last year, Union Minister Dr Jitendra Singh announced an integrated strategy to achieve ‘TB Mukt Bharat’ following PM Modi’s call at the One World TB summit. The pilot phase of the InTGS has already started, having completed Whole Genome Sequencing (WGS) of 182 TB strains. This is the joint initiative between the Ministry of Science & Technology and the Ministry of Health & Family Welfare, led by the Department of Biotechnology. DBT, ICMR, CSIR and other R&D institutes are part of the consortium targeting WGS of 32,500 TB strains. New initiatives include AYUSH interventions, drug resistance mapping using genomics and AI, and innovative blood bag technology. In 2022, the “Dare2eraD TB” programme was launched by DBT on World TB Day.
The mission of TB Alliance
Tuberculosis, often regarded as a forgotten pandemic, remains a formidable public health challenge, especially in low and middle-income countries. Eradicating TB in LMICs requires global cooperation and sustained commitment. Despite being a preventable, treatable, and curable disease, tuberculosis continues to be one of the most under-reported and underrated chronic diseases worldwide. This is a distressing reality considering that TB remains a significant cause of illness and death for many individuals.
One of the key aspects in combating TB is vaccination. The only existing TB vaccine, known as BCG (Bacillus Calmette-Guerin), was developed way back in 1921. It is mandatory in most countries around the world for infants to receive the BCG vaccine at or soon after birth. This vaccination aims to protect them from the most severe forms of TB including TB meningitis during childhood. However, its long history and widespread usage, it is crucial to critically evaluate the effectiveness and impact of the BCG vaccine in preventing TB. As global health experts continue their efforts to address this persistent disease, it becomes evident that more needs to be done beyond relying solely on a vaccine that has been in use for almost a century. It is imperative for governments, healthcare systems, and international organisations to prioritise comprehensive strategies that go beyond vaccination alone. This includes raising awareness about TB symptoms, improving access to diagnostic tools and treatment options, as well as implementing effective public health measures to control its spread. National and international organisations must prioritise funding and resources, supporting local initiatives aimed at improving health infrastructure, public awareness, and access to essential services.
The efforts of organisations like CSIR, ICMR, DBT and DST play a crucial role in advancing research and innovation in prevention, diagnostics, and treatment,. The collaboration among BRICS nations demonstrates that the fight against TB requires a multifaceted approach that addresses the complex interplay of health crises. As the world navigates post-pandemic recovery, rekindling focus on TB is essential to ensure a healthier future for vulnerable populations and to close the chapter on this persisting global health issue. A collective effort is required to combat TB, and the time for action is now. TB knows no borders, and its persistence is a stark reminder that cooperative and cohesive efforts are needed for making headway in tackling this disease. Collaborative approaches, coordination, and comprehensive strategies are necessary to turn this tide effectively.
(The authors are Sr Scientist at CSIR-National Institute of Science Communication and Policy Research (CSIR-NIScPR), New Delhi, and former Head & Adviser International Cooperation, Department of Science and Technology, New Delhi, respectively)

