Scalpel to Console
 In gynaecology, robotic surgery has transformed women’s healthcare. It addresses the limitations of traditional minimally invasive surgeries, such as laparoscopic and vaginal techniques, particularly in areas that are anatomically challenging to access.
In gynaecology, robotic surgery has transformed women’s healthcare. It addresses the limitations of traditional minimally invasive surgeries, such as laparoscopic and vaginal techniques, particularly in areas that are anatomically challenging to access.
By Dr Pakhee Aggarwal
The birth of surgical robotics is nothing short of science fiction. It dates back to the 1970s when the National Aeronautics and Space Administration (NASA) commissioned a military project funded by the Defense Advanced Research Projects Agency (DARPA). The aim was to replace the physical presence of surgeons and provide care to astronauts and soldiers in battlefields. From that day to more than five decades later, surgical robotics has come a long way. The first robotic surgery was performed by the industrial robot PUMA® (Programmable Universal Machine for Assembly) in 1985. This was a stereotactic brain biopsy using fixed anatomical landmarks. These early robots, known as first-generation robots, were capable of performing image-guided precision tasks.
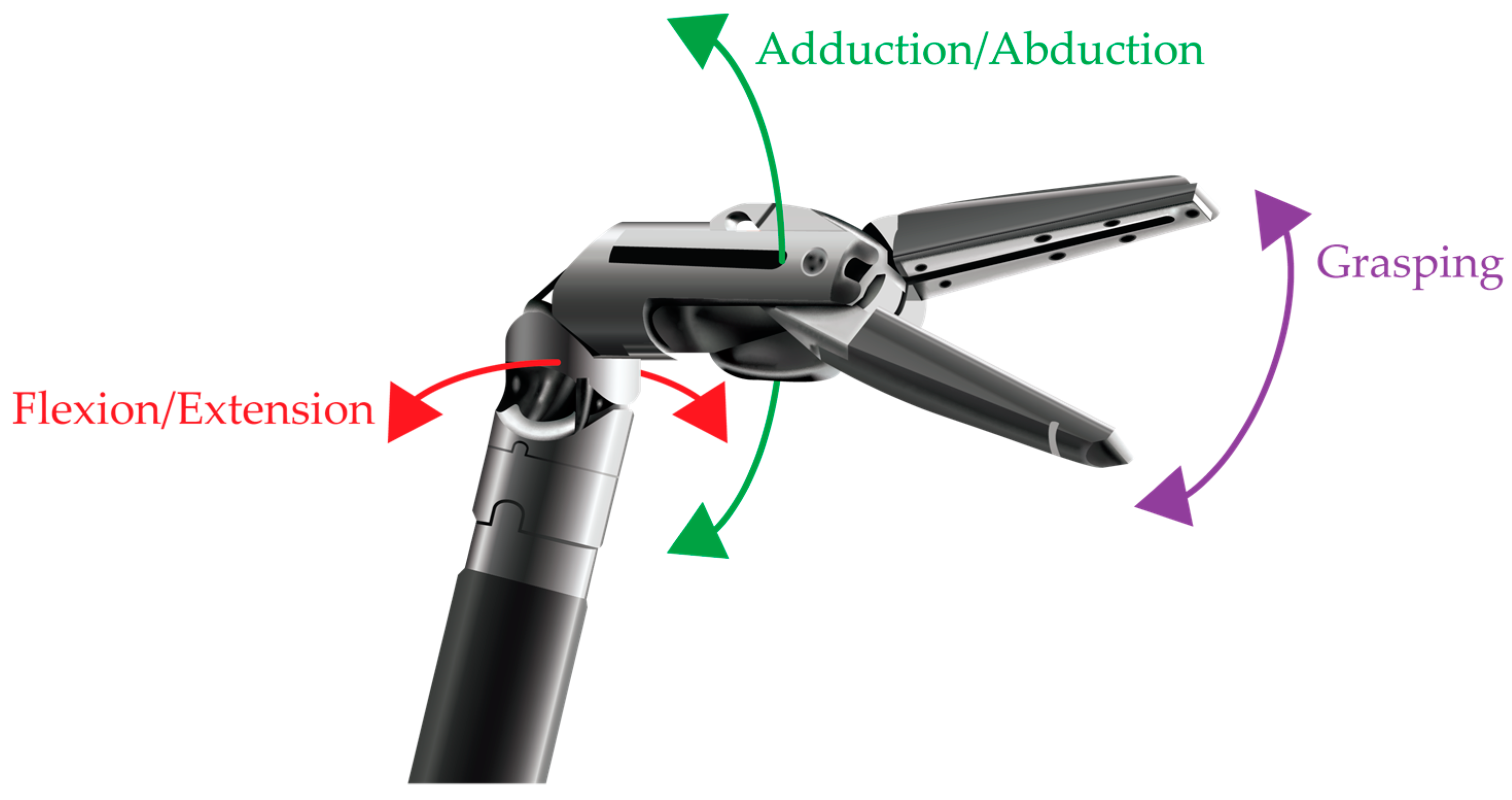
The word “robot” was coined in 1921, derived from the Czech word rabota, meaning labourer. The second and current generations of surgical robots work in a “master-slave” configuration, where the surgeon (master) controls the robotic arms (slave). These robotic arms possess multiple degrees of flexibility, even more than the human hand, allowing them to perform intricate visceral surgeries, where organs are not static but in constant motion.
 Robotic surgery is essentially computer-assisted surgery, designed to enhance precision and safety during operations. The autonomy of robots typically decreases with their proximity to the patient. A surgical robot, such as those used in gynaecology, operates entirely under the surgeon’s control without any autonomy.
Robotic surgery is essentially computer-assisted surgery, designed to enhance precision and safety during operations. The autonomy of robots typically decreases with their proximity to the patient. A surgical robot, such as those used in gynaecology, operates entirely under the surgeon’s control without any autonomy.
In gynaecology, as in other specialties like urology, general surgery, ENT, and cardiac surgery, robotic systems were developed to overcome the limitations of minimally invasive surgery, which struggles in deep-seated areas difficult to access with conventional techniques. Robotic systems also extend the capabilities of surgeons performing open surgeries.
This technology can be seen as a hybrid technique combining the best features of both open and laparoscopic surgery. It allows natural hand movements to be replicated through less-than-centimetre-wide incisions. Robotic surgery has been in practice for over two decades, ever since the FDA approved the da Vinci Surgical System® in 2000.
The technology has seen continuous advancements, and now fifth-generation surgical robots are in use, significantly enhancing surgical precision and safety. The surgeon operates these advanced robotic arms from a workstation, sitting at a distance from the patient, making it a form of telesurgery. This contrasts with conventional surgery, where the surgeon is physically present beside the patient. Importantly, the robotic system does not function autonomously but serves as an instrument handling system facilitating the surgeon’s work.
Robotic technology enhances both surgeon and patient experiences. Surgeons have full control over four robotic arms simultaneously—double the number of human hands traditionally used in surgery. Let’s delve into how robotic technology surpasses conventional surgical methods, whether open, laparoscopic, vaginal, or natural-access approaches.
The types of gynaecological surgeries frequently performed using robotic systems include hysterectomies (for fibroids or abnormal bleeding), radical hysterectomies (for cancer treatment), myomectomies (for fertility preservation in fibroids), endometriosis surgery (for pain relief and fertility), ovarian cystectomies or oophorectomies (for ovarian tumours), sacrocolpopexies (for pelvic organ prolapse), tubal recanalisation (for fertility restoration), and fistula repairs. Traditionally, these procedures were carried out through open surgery or later by laparoscopic or vaginal methods, as the benefits of minimally invasive techniques became evident.
 However, challenges arise when the surgical site is difficult to access due to adhesions, distorted anatomy, multiple previous surgeries, or obesity. Open surgery poses limitations, including delayed healing from large incisions, increased risks of hernias, more post-operative adhesions, higher blood loss requiring transfusions, and longer hospital stays. Patients also face prolonged recovery periods and time off work. Additionally, open surgery carries risks such as infections and, rarely, surgical errors like retained sponges in complex procedures.
However, challenges arise when the surgical site is difficult to access due to adhesions, distorted anatomy, multiple previous surgeries, or obesity. Open surgery poses limitations, including delayed healing from large incisions, increased risks of hernias, more post-operative adhesions, higher blood loss requiring transfusions, and longer hospital stays. Patients also face prolonged recovery periods and time off work. Additionally, open surgery carries risks such as infections and, rarely, surgical errors like retained sponges in complex procedures.
Laparoscopic surgery addresses some of these issues but introduces its own challenges. Traditional laparoscopic instruments have limited range and operate in only two dimensions, lacking the wrist-like flexibility of human hands. This makes complex movements and suturing more difficult, requiring significant skill and effort from surgeons. Furthermore, conventional cameras used in laparoscopic surgery reduce depth perception and, consequently, surgical precision. Prolonged laparoscopic procedures can also cause strain on the surgeon’s neck and shoulders.
Despite these limitations, laparoscopic surgery, which has been practiced for nearly 50 years, offers faster recovery compared to open surgery. Nevertheless, robotic surgery represents a revolution in minimally invasive techniques, addressing the challenges and limitations of both traditional approaches.
The robotic platform offers several advanced features, including binocular vision for the surgeon with stable camera control, ease in manipulating the field of vision, Endowrist® instrumentation technology, high-definition 3D vision, 10x magnification, precision in incisions, effortless suturing, and the ability to sit comfortably while operating. The multi-tasking capabilities of robotic instruments replicate high surgical standards consistently.
Robotic technology comprises three main components: the surgeon console, patient cart, and vision cart. The surgeon console serves as the primary surgical unit, operated by the surgeon using hand controls or masters. These controls translate the surgeon’s movements into electrical signals that guide the robotic instruments. Foot switches and pedals allow the surgeon to control the camera, monopolar and bipolar cautery, and an additional robotic arm in an ergonomically efficient manner. Moreover, features such as motion scaling and tremor filtration enable seamless movements, providing unparalleled surgical precision.
Endowrist® technology enhances dexterity, allowing the robotic instruments to rotate 360 degrees (seven degrees of freedom), compared to the human wrist’s 270-degree rotation. This capability proves invaluable for dissection or suturing at challenging angles in complex cases. Despite their compact size, robotic instruments, including forceps, graspers, bipolar and monopolar cautery tools, and needle drivers, perform functions equivalent to conventional instruments.
For patients, these advancements translate into numerous benefits: significantly less pain and scarring, reduced postoperative discomfort, minimal blood loss and need for transfusions, lower infection risks, shorter hospital stays, reduced medication use, quicker recovery times, smaller incisions for improved cosmetic outcomes, and overall higher satisfaction rates.
From a surgeon’s perspective, robotic technology offers considerable advantages, such as a three-dimensional stereoscopic view, magnification, improved ergonomics, reduced surgical fatigue, and fewer errors. These benefits are particularly pronounced in complex cases involving obesity, pelvic adhesions, large masses, prior surgeries, anaemia, or other medical comorbidities.
Robotic Surgery in Gynaecology
Robotic surgery has shown its superiority in specific gynaecological scenarios, such as managing endometrial cancer and preserving fertility.
Endometrial Cancer
Patients with endometrial cancer are often obese and have multiple comorbidities, such as diabetes and hypertension. Conventional open surgery in such cases leads to prolonged healing times and increased risks of complications, including deep vein thrombosis, wound infections, and resuturing. Robotic surgery, combined with enhanced recovery protocols, facilitates early mobilisation and quicker bowel function restoration, reducing complication risks. Additionally, robotic technology enables targeted mapping and removal of sentinel lymph nodes, which significantly lowers the risk of lymphedema—by up to tenfold—without compromising oncological outcomes. As a result, international guidelines frequently recommend robotic surgery for endometrial cancer.
Fertility Preservation
For young women with fibroids or ovarian cysts, robotic surgery offers unmatched precision and magnification, which are critical for distinguishing normal tissue from diseased tissue. This ensures organ preservation with minimal collateral damage. This is especially advantageous when fibroids are located in challenging areas, such as the posterior wall or cervical region, or when intricate suturing is required. Similarly, robotic technology is beneficial for treating ovarian cysts, such as dermoids and endometriomas, safeguarding ovarian reserves and improving fertility outcomes.
 Robotic surgery is applicable to a wide range of gynaecological conditions, including cancers. However, it offers limited advantages over laparoscopy in certain cases, such as diagnostic procedures for infertility or cancer assessment, where cost-effectiveness becomes a concern. Despite its many benefits, robotic surgery cannot replace surgical expertise and experience, as the system is entirely controlled by the surgeon. Additionally, the lack of haptic feedback requires a learning curve, particularly for beginners. In India, the availability of robotic surgery may also be influenced by insurance coverage, limiting access for some patients.
Robotic surgery is applicable to a wide range of gynaecological conditions, including cancers. However, it offers limited advantages over laparoscopy in certain cases, such as diagnostic procedures for infertility or cancer assessment, where cost-effectiveness becomes a concern. Despite its many benefits, robotic surgery cannot replace surgical expertise and experience, as the system is entirely controlled by the surgeon. Additionally, the lack of haptic feedback requires a learning curve, particularly for beginners. In India, the availability of robotic surgery may also be influenced by insurance coverage, limiting access for some patients.
Guidelines and Future Prospects
Several international bodies, including the American College of Obstetrics and Gynecology, have issued guidelines on robotic surgery. These emphasise the importance of comprehensive patient counselling, covering indications for surgery, risks and benefits of robotic techniques compared to alternatives, and the surgeon’s experience with robotic procedures. Surgeons are advised to master abdominal and laparoscopic techniques for specific procedures before transitioning to robotic approaches.
The future of robotic surgery is promising, with advancements such as single-incision surgery, integrated imaging, and 3D reconstruction already aiding surgical planning. Emerging technologies like augmented reality and remote surgery are also on the horizon, paving the way for further innovation in this field.
(The author is Senior Consultant Gynaecology Oncology & Robotic Surgery, Indraprastha Apollo Hospitals, New Delhi)

